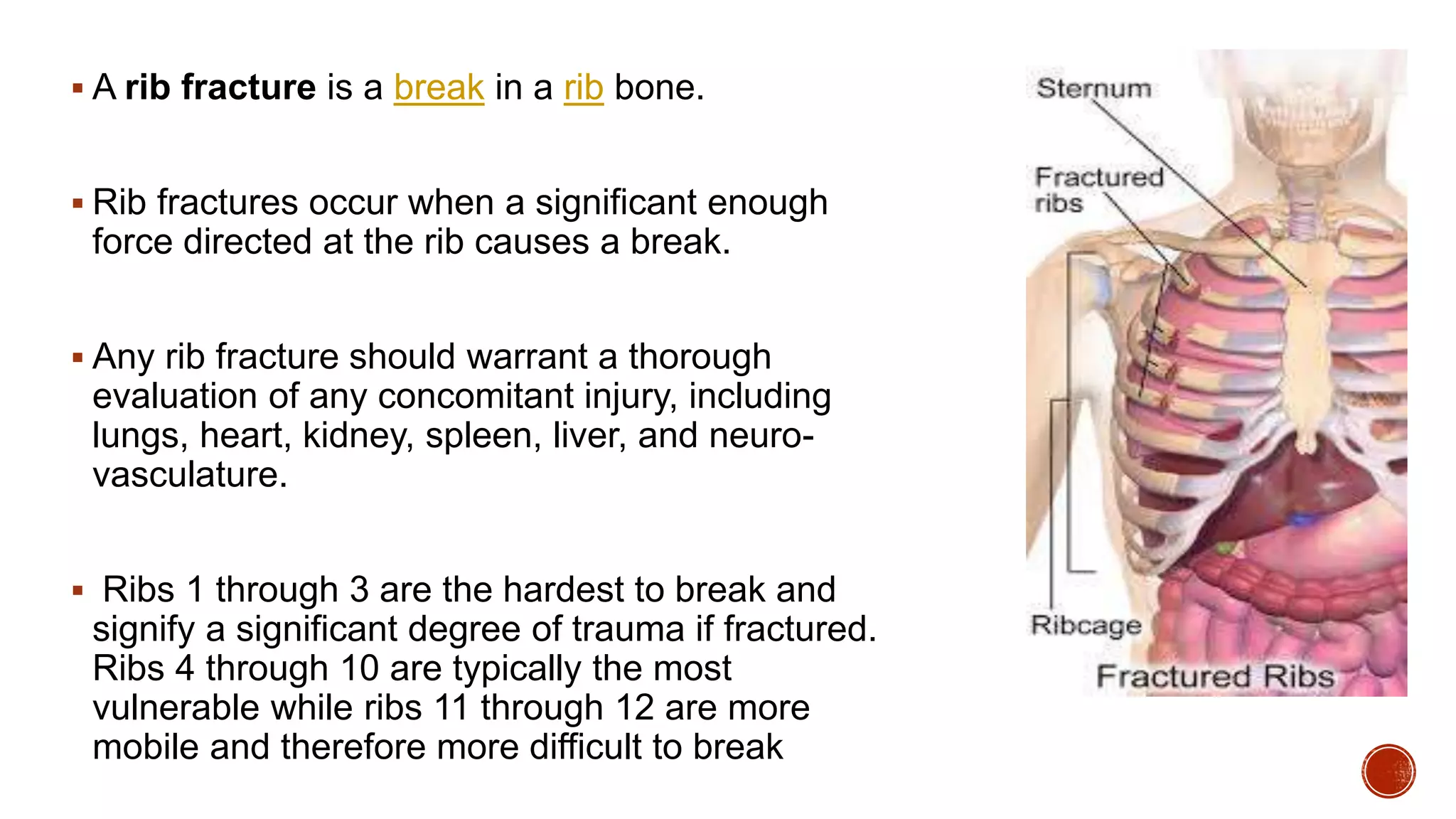
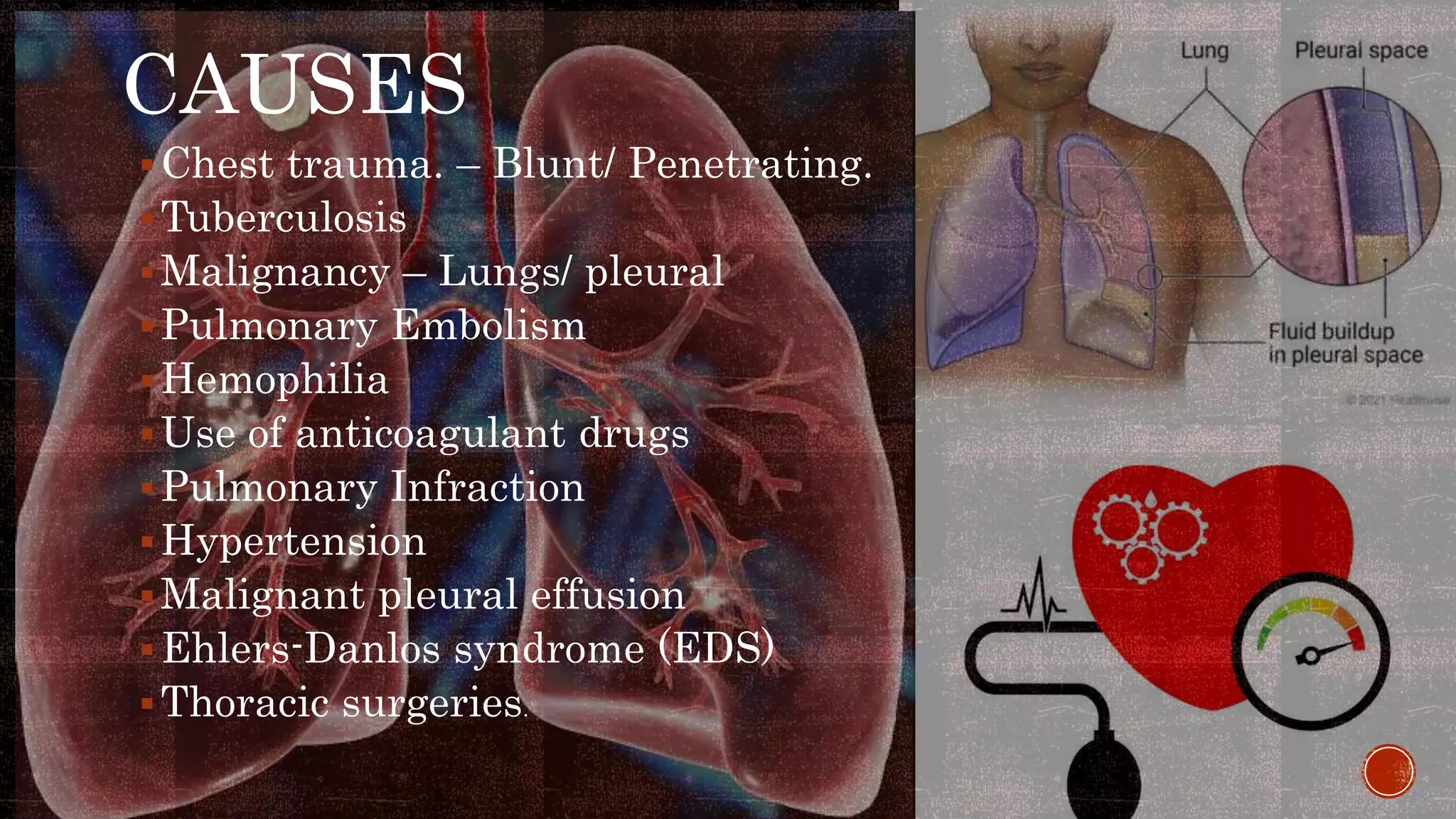
This document discusses chest injuries and their management. It begins by introducing chest trauma as life-threatening due to injuries to the heart, lungs, and blood vessels in the chest. It then defines chest injury and provides epidemiological data showing thoracic trauma is a leading cause of trauma deaths. Specific injuries discussed in detail include rib fractures, flail chest, pneumothorax, and hemothorax. For each injury, the document covers causes, signs/symptoms, diagnostic tests, and treatment approaches including analgesics, ventilator support, chest tube insertion, and surgery. Nursing assessments and interventions are also reviewed.