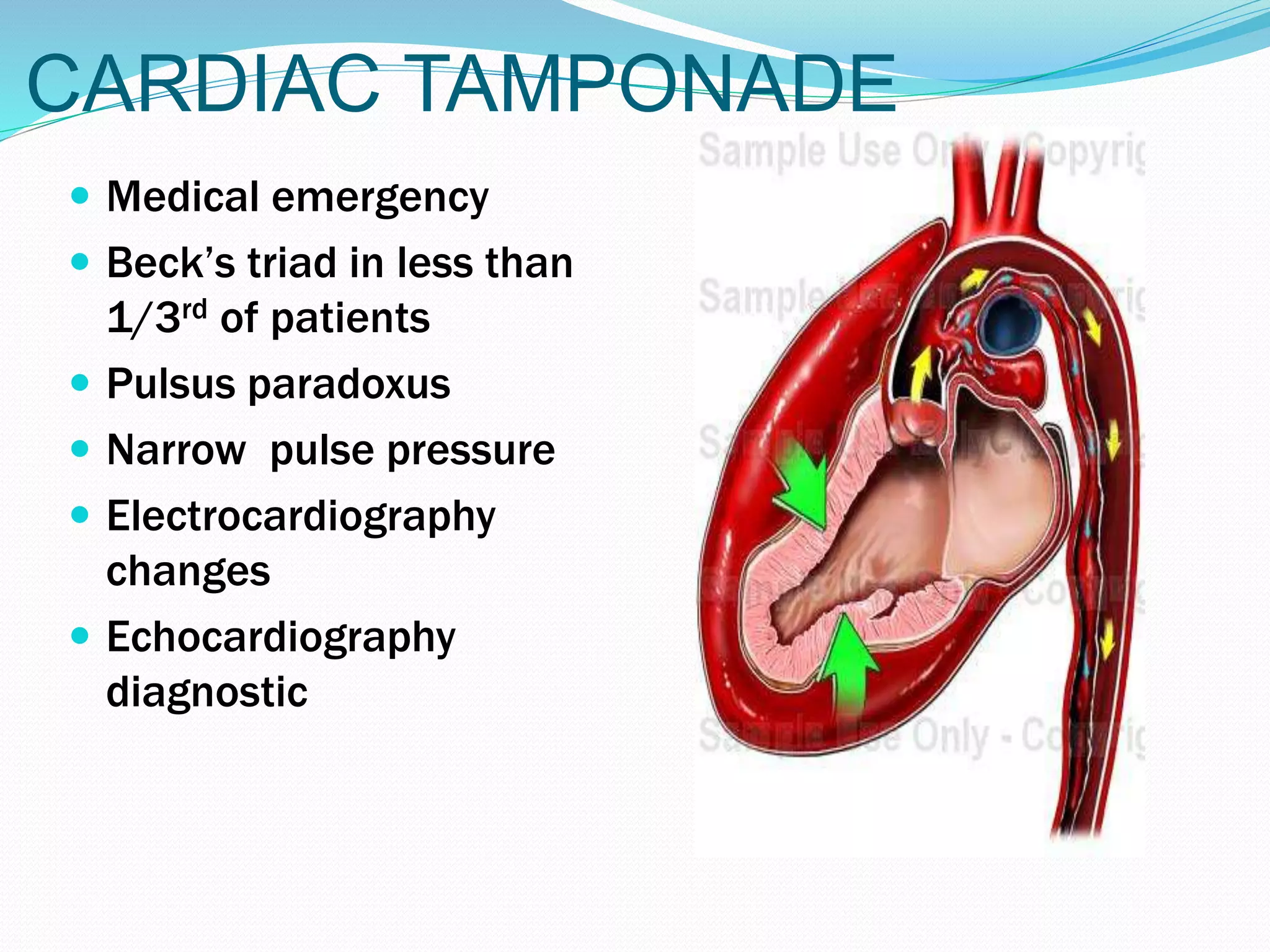
This document discusses the management of chest injuries. It begins with an introduction stating that chest trauma is a significant cause of morbidity and mortality worldwide. It then covers the epidemiology, relevant anatomy, causes, pathophysiology, investigations, management, and complications of various chest injuries. The pathophysiology section describes the mechanisms and types of injuries that can occur to the chest wall, pleura, lungs, heart, and major vessels. Management involves following ATLS protocols, administering analgesics and antibiotics, and performing procedures such as tube thoracostomy or thoracotomy when needed to treat injuries such as hemothorax, flail chest, or cardiac tamponade. Complications include wound infections, dehiscence,