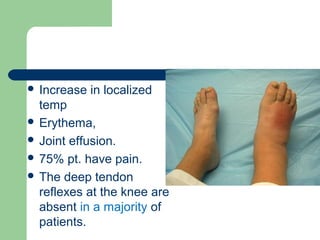
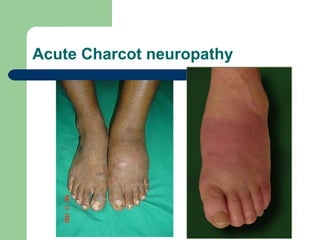
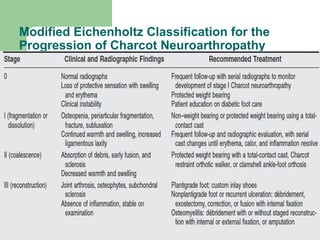
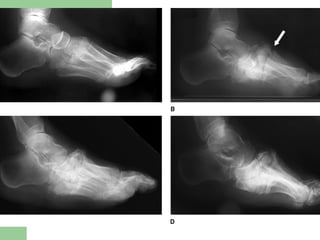
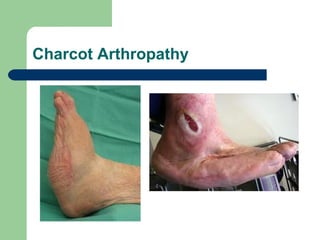
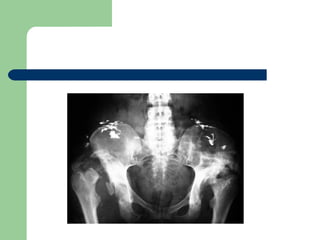
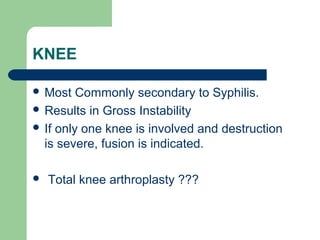
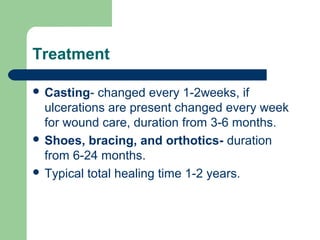
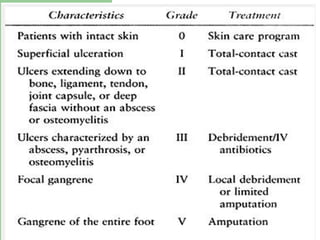
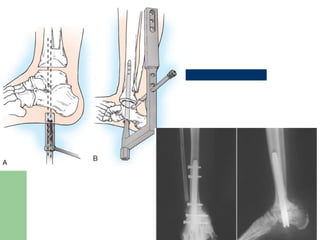
Neuropathic arthropathy, also known as Charcot arthropathy, is a condition characterized by progressive joint destruction and deformity caused by loss of sensation in the joints. It is most commonly seen in patients with diabetes or neurological disorders. The main theories for its pathophysiology are neurotrauma from repetitive micro-injuries without pain perception, and neurovascular changes that increase bone resorption. Treatment involves initial casting to immobilize the joint, followed by bracing, orthotics, and immobilization over the course of 1-2 years to allow healing. Surgical options like fusion or reconstruction may be used for advanced cases or deformity correction.