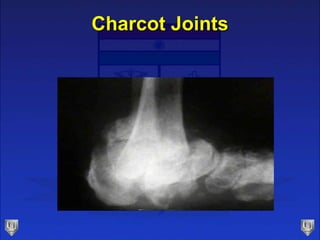
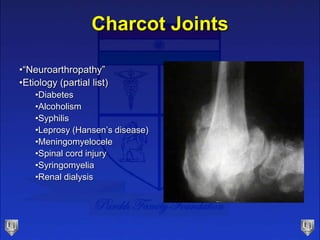
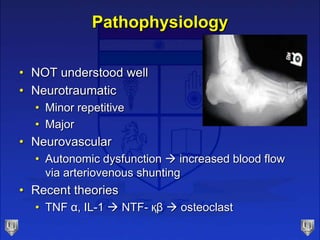
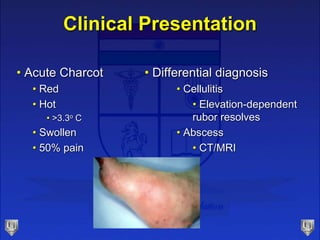
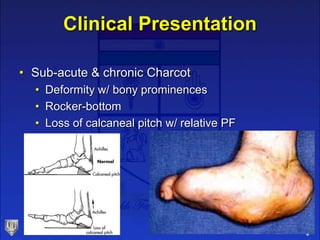
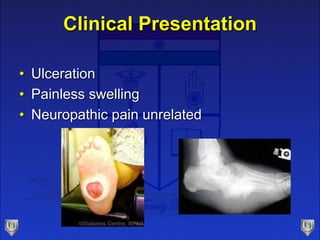
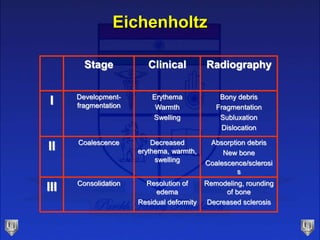
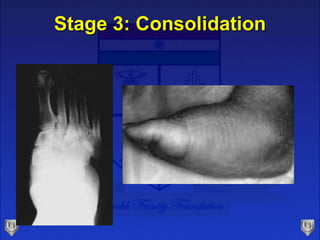
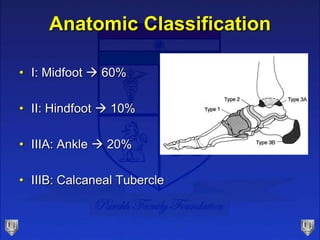
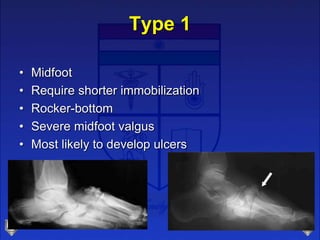
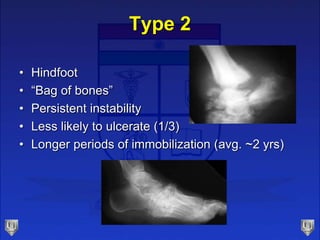
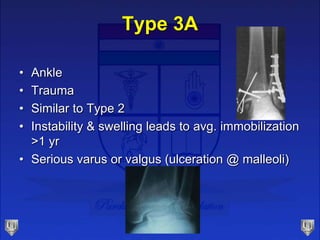
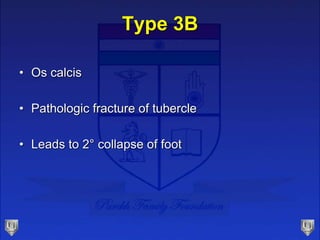
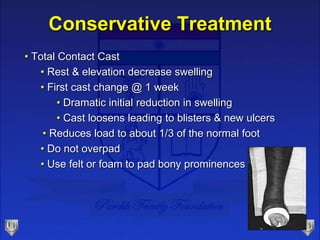
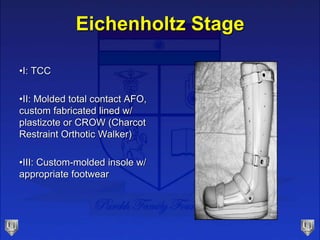
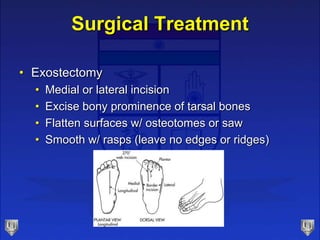
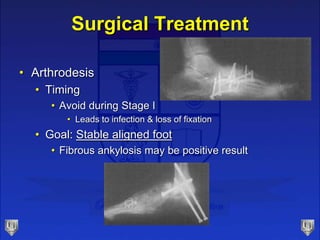
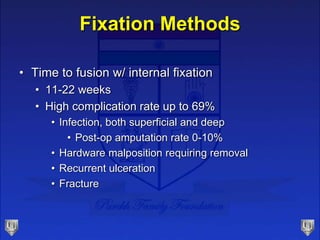
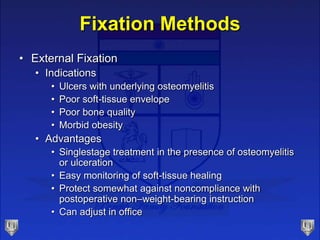
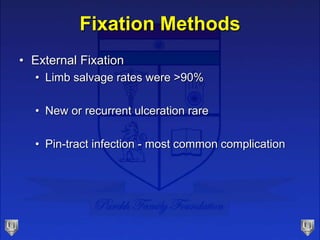
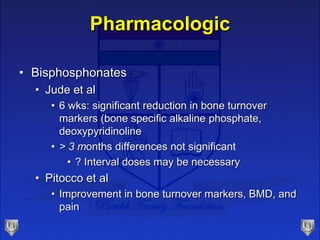
Charcot foot and ankle, also known as neuropathic arthropathy, is a progressive destructive disease affecting bones and joints in people with sensory neuropathy. It is most commonly seen in the foot and ankle. The main causes are diabetes, alcoholism, syphilis, leprosy, spinal cord injury, and renal dialysis. It results from repetitive mechanical trauma to an insensate foot. Treatment involves immobilization with a total contact cast to stabilize the foot during healing, which can take many months or years. Surgery may be needed for severe deformity or non-healing ulcers.