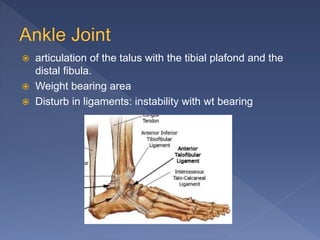
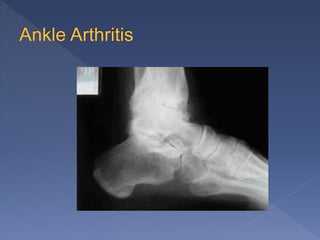
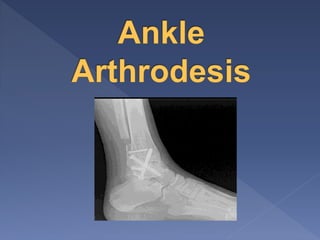
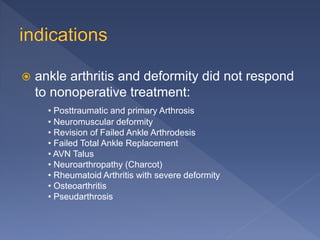
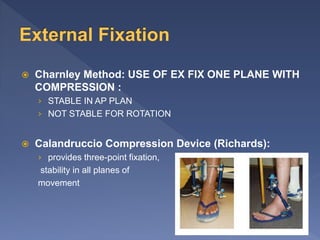
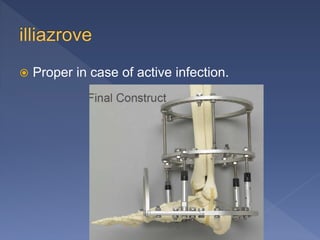
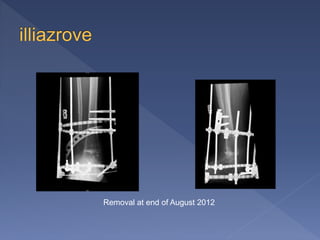
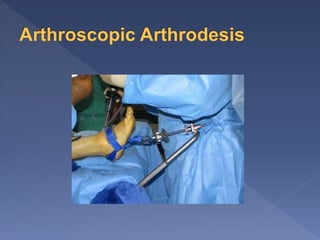
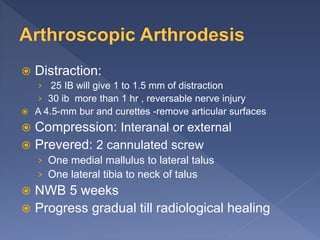
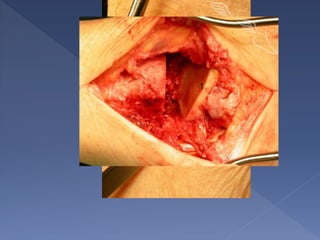
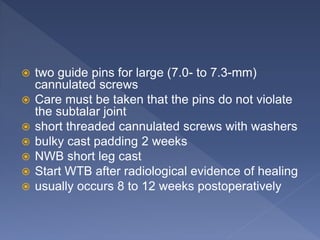
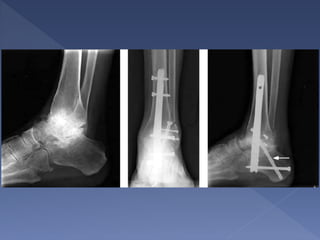
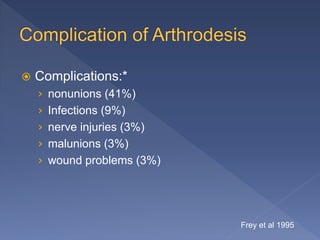
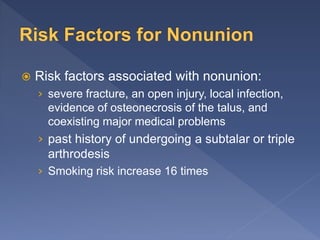
This document discusses ankle arthritis and its treatment options. It provides details on the anatomy of the ankle joint and common causes of ankle arthritis, including post-traumatic, inflammatory, degenerative, and avascular necrosis. Non-surgical treatments for ankle arthritis like orthotics, bracing, injections and activity modification are outlined. Surgical options covered include arthroscopic debridement, ankle fusion (arthrodesis), and total ankle replacement. Specific techniques for ankle fusion using both external and internal fixation are summarized. Complications associated with ankle fusion like nonunion are also mentioned.