Charcot osteoarthropathy is a progressive deterioration of weight-bearing joints caused by neuropathy. It most commonly affects the feet and ankles of diabetic patients. Treatment involves immobilization with casting in early stages to prevent fractures and deformity. Later stages may require surgical fusion of affected joints. Arthrodesis fuses bones to stabilize severe deformities and relieve pain, though it limits ankle motion and increases stress on other joints. Multiple techniques exist including internal fixation with screws or plates. Bone grafting aids fusion while bracing post-surgery protects new bone formation.













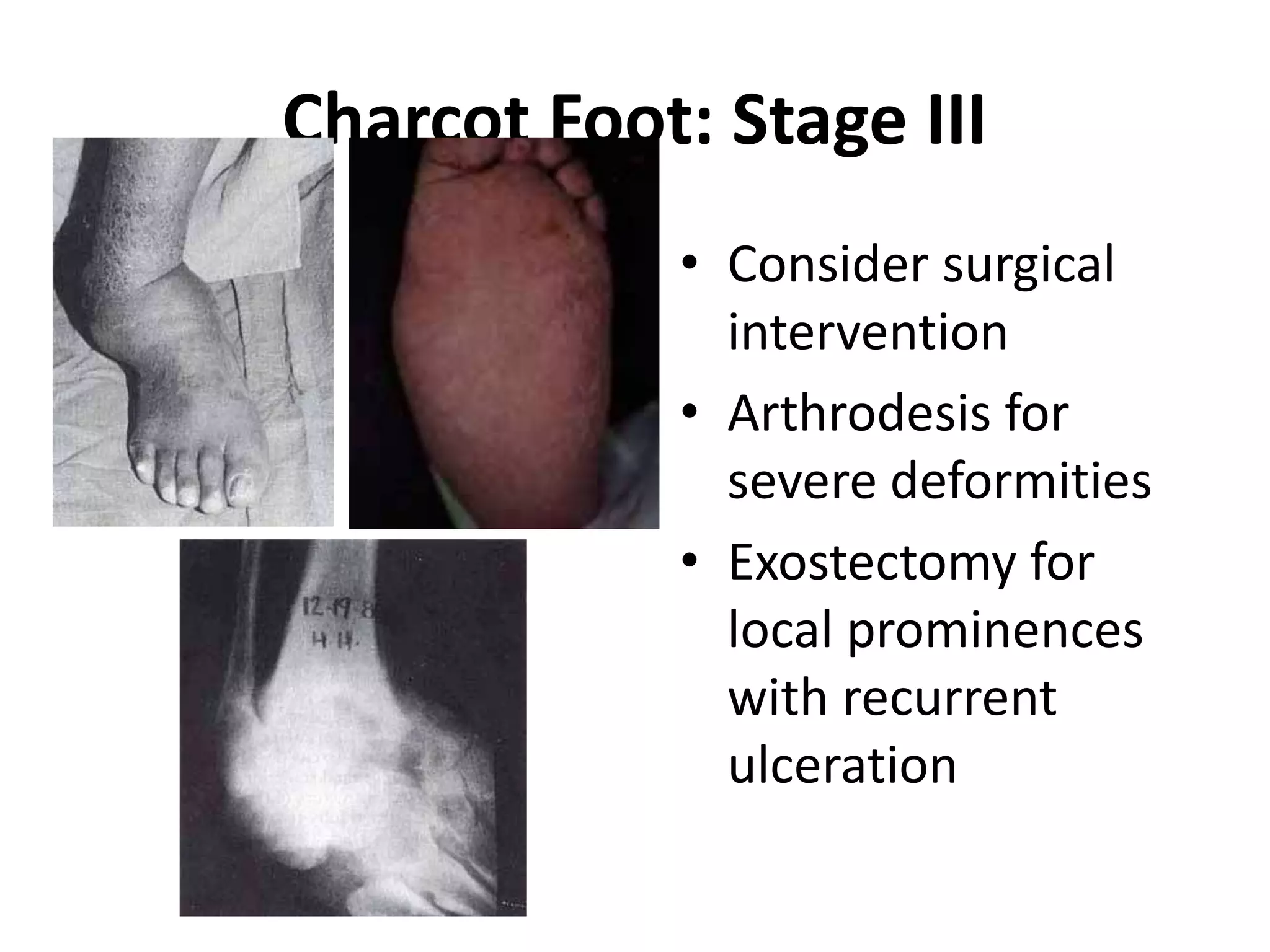
![Charcot Foot: Stage I
[Fragmentation]
• Initial presentation = hot,
swollen, painless foot! Early
radiographs negative!
• No fever, malaise; normal
WBC!
• Patient usually walks into
clinic
• Hyperemia precedes bony
destruction](https://image.slidesharecdn.com/charcotjointmethodsofarthrodesis-230123144233-255781f7/75/Charcot-Joint-Methods-of-Arthrodesis-pptx-14-2048.jpg)






![Treatment
• Stage 1:
• Immediate weight
bearing
protection!
Severe/bilateral =
bed rest!
Wheelchair
mobility!
Crutch walking [if
good balance]!
Total Contact
Casting [TCC]](https://image.slidesharecdn.com/charcotjointmethodsofarthrodesis-230123144233-255781f7/75/Charcot-Joint-Methods-of-Arthrodesis-pptx-22-2048.jpg)


![Charcot Foot: Stage II
[Coalescence]
• Maintain external foot
contours while bone
Reconstitutes.
• Controlled weight
bearing believed to
facilitate healing.
• Wean from TCC to AFO
• Custom shoe, if foot is
deformed](https://image.slidesharecdn.com/charcotjointmethodsofarthrodesis-230123144233-255781f7/75/Charcot-Joint-Methods-of-Arthrodesis-pptx-25-2048.jpg)