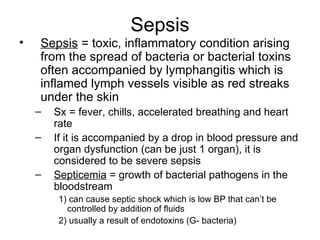
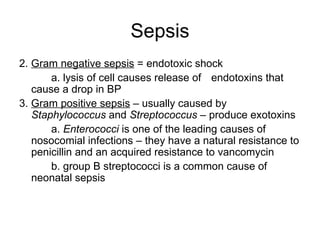
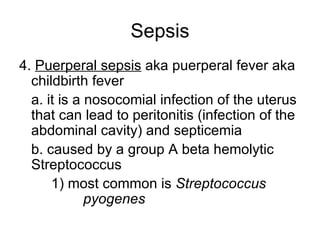
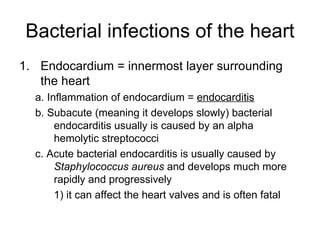
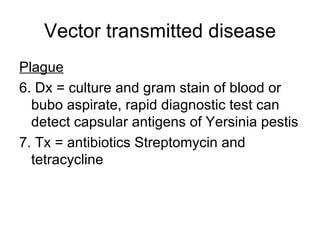
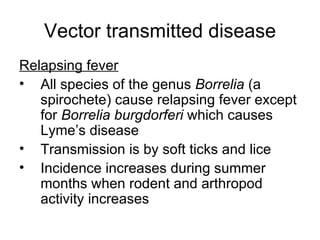
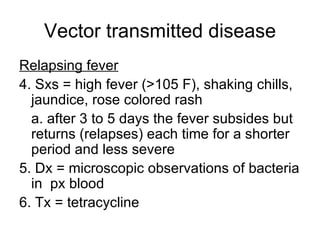
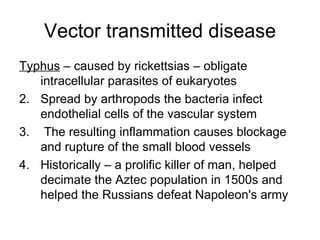
This document provides an overview of diseases that can affect the cardiovascular and lymphatic systems. It discusses several types of infections including sepsis, bacterial infections of the heart, tularemia, brucellosis, anthrax, gangrene, diseases caused by animal bites/scratches, plague, and relapsing fever. For each disease, it describes the causative pathogen, transmission, signs and symptoms, pathogenesis, diagnosis, and treatment.