The document discusses the anatomy, histology, epidemiology, clinical features, diagnosis, staging, and treatment of nasopharyngeal carcinoma (NPC). Key points include:
- NPC originates from the epithelial lining of the nasopharynx.
- It has a strong association with Epstein-Barr virus.
- Risk factors include genetic predisposition and environmental exposures like salted fish consumption.
- Common symptoms are cervical lymphadenopathy, epistaxis, ear symptoms, and neurological deficits.
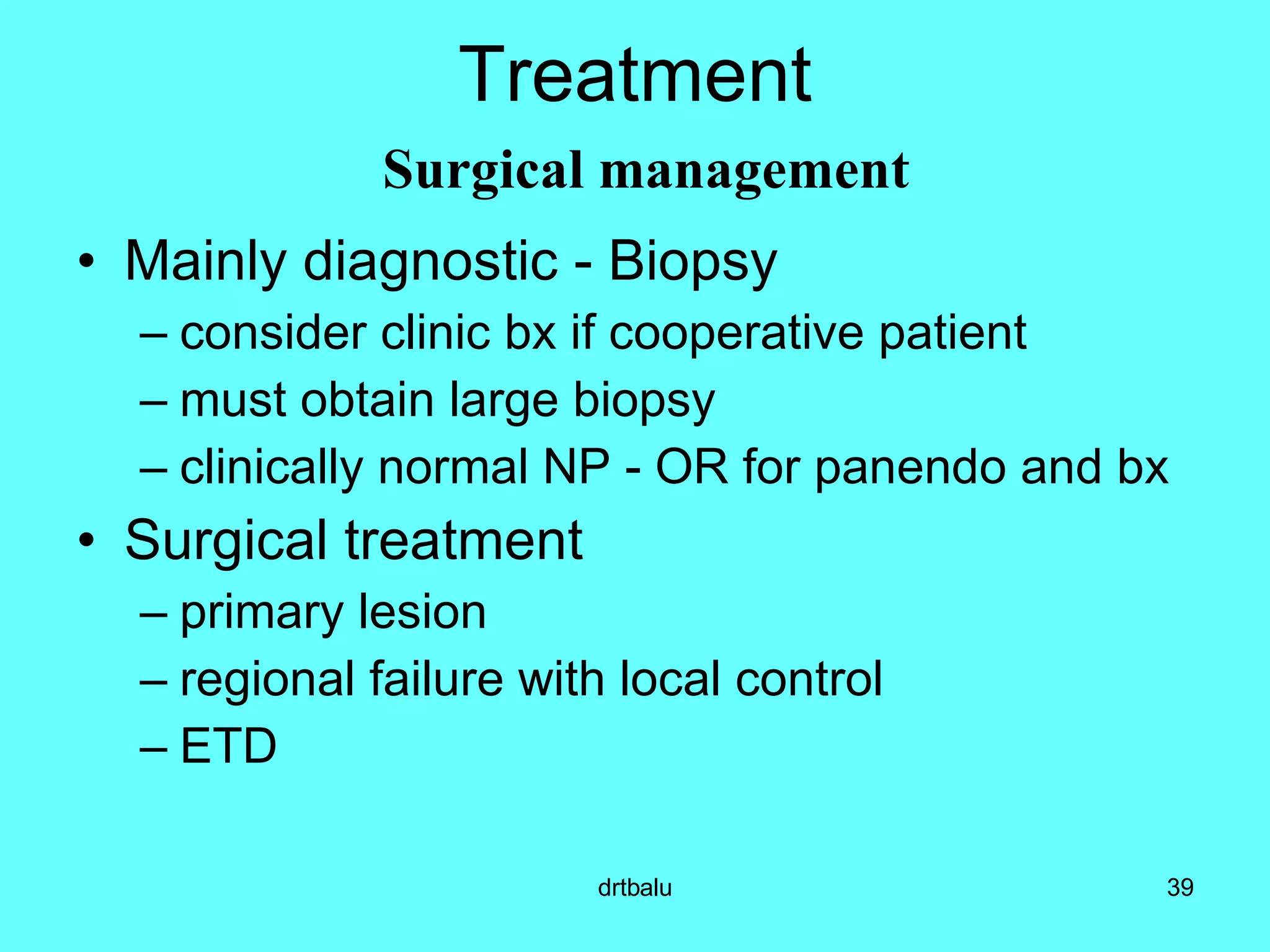
- Diagnosis involves biopsy and serological testing for EBV markers.
- Staging systems consider tumor size, node involvement, and serological factors.
- Primary treatment is radiotherapy,