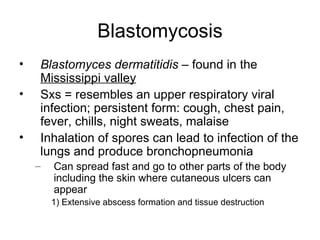
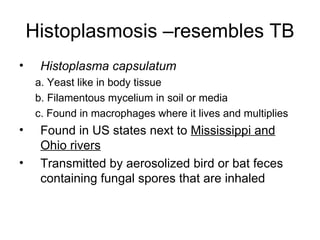
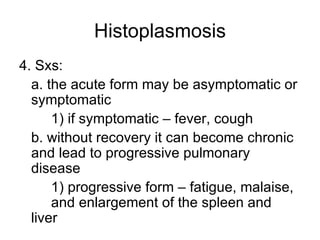
The document provides an overview of several diseases that affect the respiratory system, including both the upper and lower tract. It discusses bacterial infections like strep throat, scarlet fever, diphtheria, pertussis, tuberculosis, and pneumococcal pneumonia. It also covers atypical pneumonia, Legionnaire's disease, and some fungal diseases. For each condition, it describes the causative pathogen, signs and symptoms, diagnosis, treatment and other relevant details.