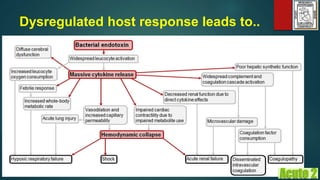
1) Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection. It is a major healthcare problem with high mortality rates, especially septic shock which has mortality rates of 50-60%.
2) The new Sepsis-3 definition defines sepsis as a life-threatening organ dysfunction caused by a dysregulated host response to infection represented by an increase of two or more points in the SOFA score.
3) Early goal-directed therapy (EGDT) is a protocol-based approach for initial resuscitation of sepsis patients. It aims to achieve specific goals for central venous pressure, mean arterial pressure, ScvO2, and other parameters within 6 hours and



![Epidemiology
Martin, G. S., Mannino, D. M., Eaton, S., & Moss, M. (2003). The
epidemiology of sepsis in the United States from 1979 through 2000.
New England Journal of Medicine, 348(16), 1546–1554.
Harrison, D. A., Welch, C. A., & Eddleston, J. M. (2006). The
epidemiology of severe sepsis in England, Wales and
Northern Ireland, 1996 to 2004: secondary analysis of a high
quality clinical database, the ICNARC Case Mix Programme
Database. Critical Care, 10(2), R42.
Brun-Buisson, C., Meshaka, P., Pinton, P., Vallet, B., EPISEPSIS
Study Group. (2004). EPISEPSIS: a reappraisal of the epidemiology
and outcome of severe sepsis in French intensive care units.
Intensive Care Medicine, 30(4), 580–588.
[1993 - 2001]...a 17%
reduction in mortality.
[1993-2001]...a
75% increase in... severe
sepsis...
Incidence
of Sepsis
Mortality
of Sepsis](https://image.slidesharecdn.com/sepsisacute2final-160822134045/85/Sepsis-2016-5-320.jpg)


























![System-based Approaches to sepsis
Early-Goal Directed Therapy
INCLUSION = SEPSIS AND [BP < 90 after fluid OR Lactate > 4]
CVP 8-12 Fluids CVP 8-12
MAP > 65 Vasopressors MAP > 65
Transfusions
Dobutamine
ScvO2 > 70%
49% mortality 33% mortality
Rivers, E., Nguyen, B., Havstad, S., Ressler, J., Muzzin, A., Knoblich, B., Peterson, E., et al. (2001). Early goal-directed therapy in the treatment of severe sepsis and septic shock. New England Journal of Medicine, 345(19), 1368–1377.
Control Intervention EGDT](https://image.slidesharecdn.com/sepsisacute2final-160822134045/85/Sepsis-2016-35-320.jpg)