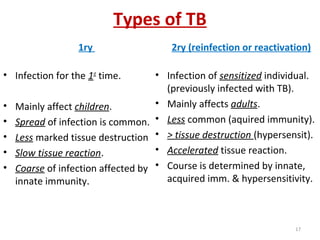
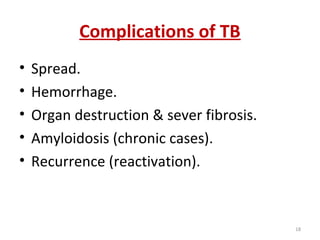
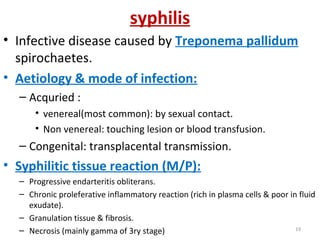
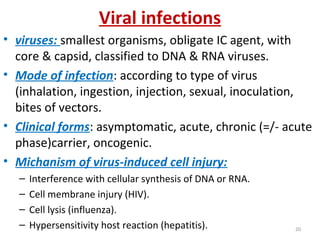
This document discusses various types of bacterial and viral infections. It defines key terms like infection, bacteraemia, toxemia, septicaemia, pyaemia, and chronic bacterial infections. It also summarizes the pathogenesis, effects, and clinical manifestations of these conditions. Tuberculosis and syphilis are discussed in further detail regarding their causative organisms, modes of transmission, tissue reactions, and complications. Viral infections are also briefly introduced.
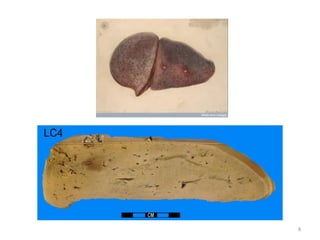
![Tissue reaction in TB
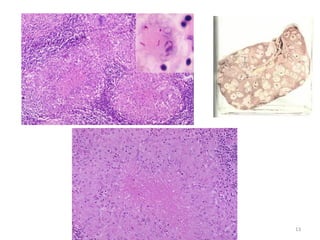
• Proliferative (the tubercle): basic lesion of TB
– Mode of formation: nutrophils, macrophages that become
epithelioid cells that fuse (Langhan’s giant cells), sensitize T
lymphocytes (aquired imm. In 10-14d) that produce lymphokines
causing macrophage stimulation & promote caseation.
– Gross: tubrcles are microscopic, when fuse give grossly small
yellow grey, soft, cheesy (caseation) nodules.
– M/P: each tubercle: caseation necrosis in the centre surrounded
by epithelioid cells, Langhan’s giant cells & lymphocytes (form a
peripheral zone).
– Michanism of caseation: cytotoxic lymphokines & ischemic
necrosis (no angiogenesis + endarteritis).
– Fate of tubercle:
• localization [(fibrosis+/- dystrophic calcifications) of small or large
(encapsulation, dormant bacilli, reactivation)] or spread acc. To immunity.12](https://image.slidesharecdn.com/19-bact-180301044350/85/19-bact-inf-12-320.jpg)