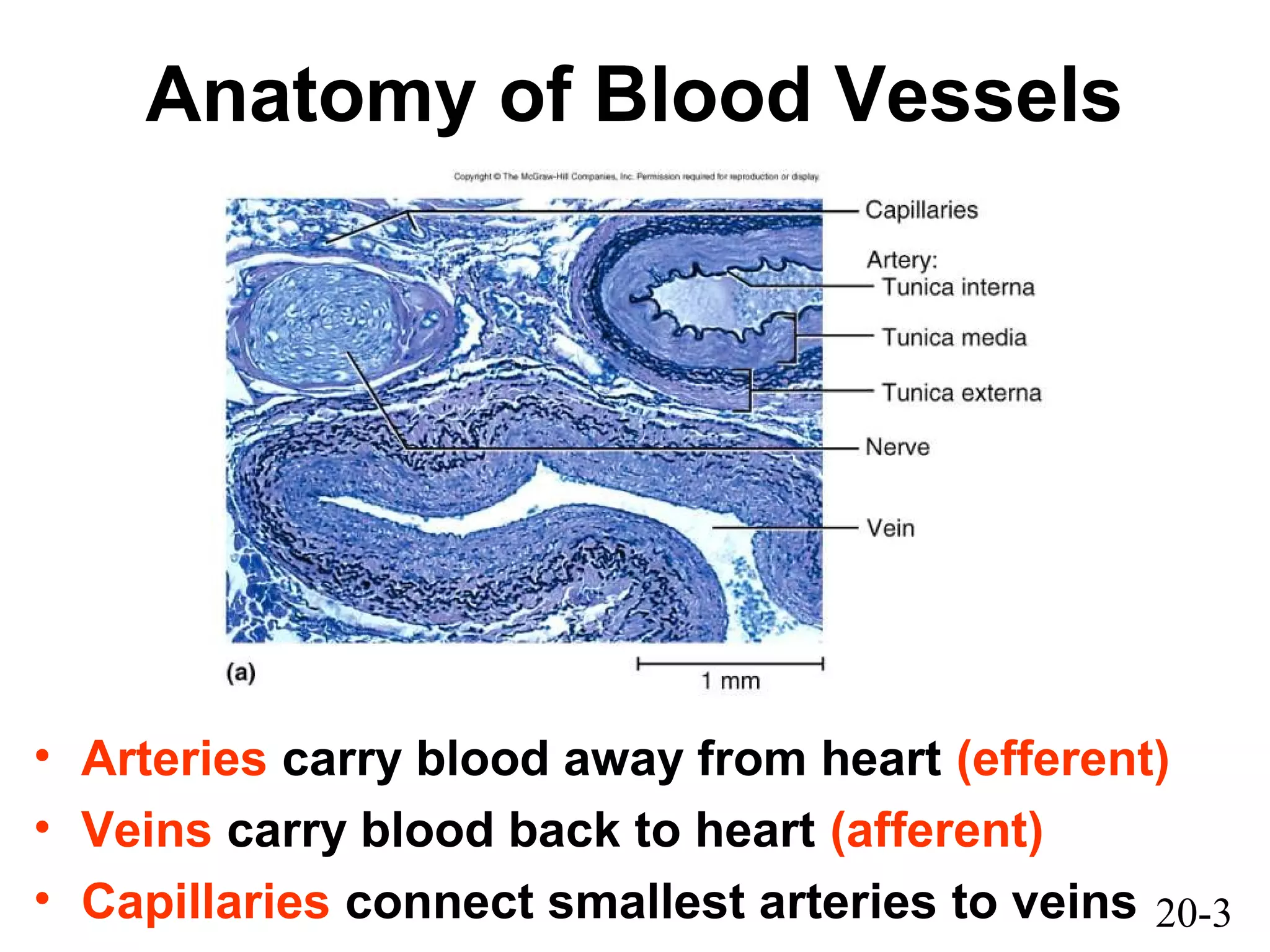
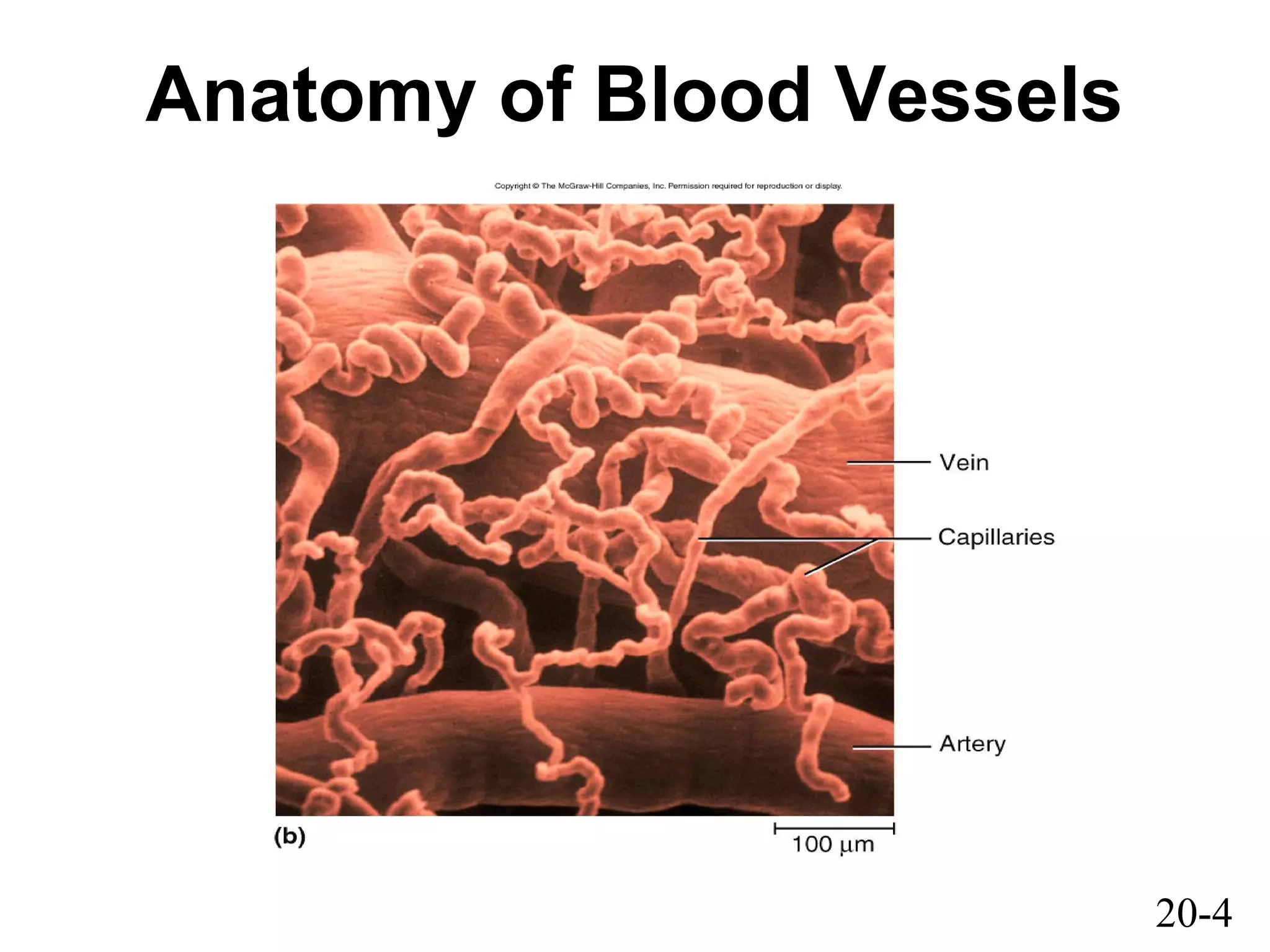
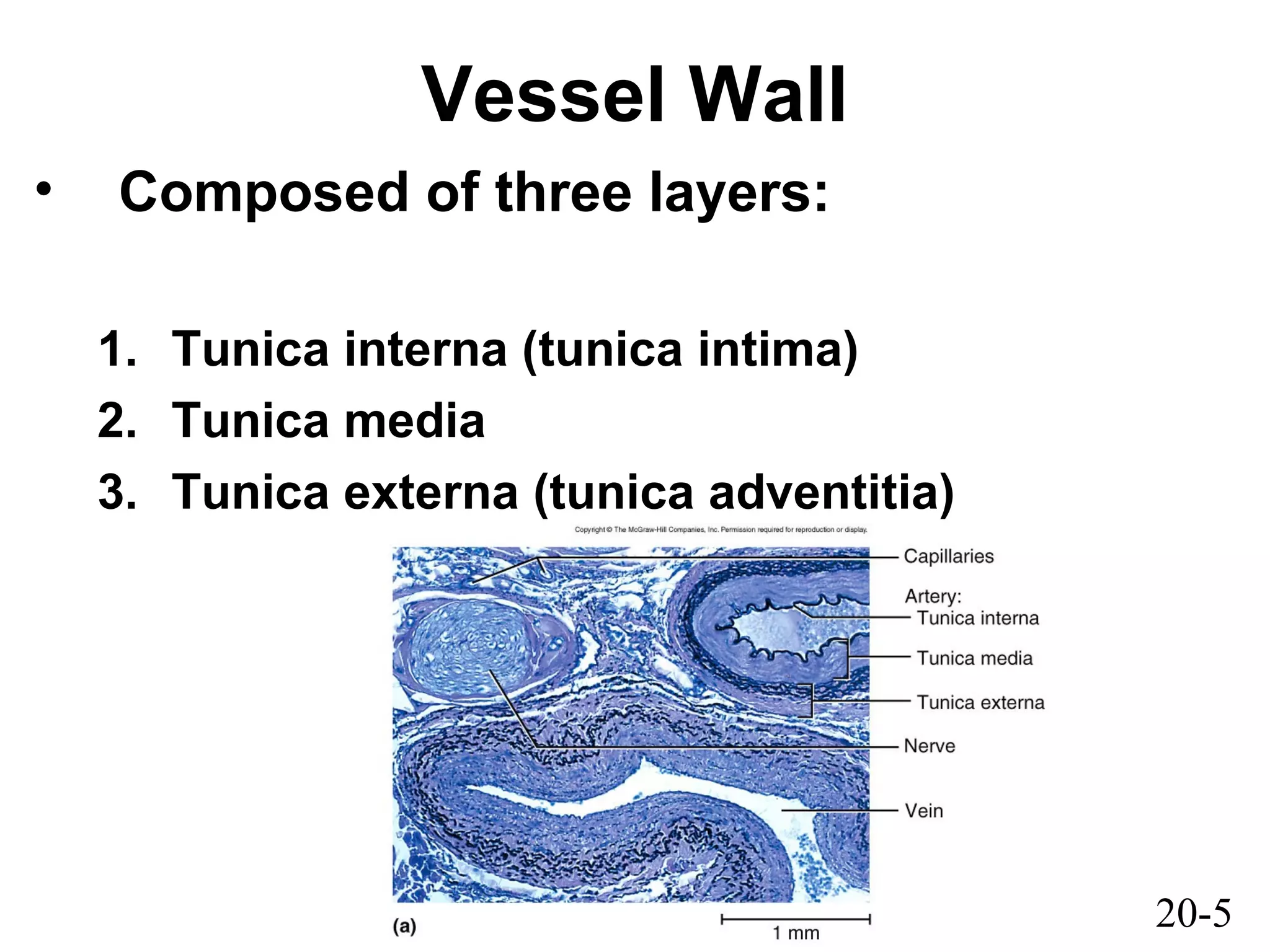
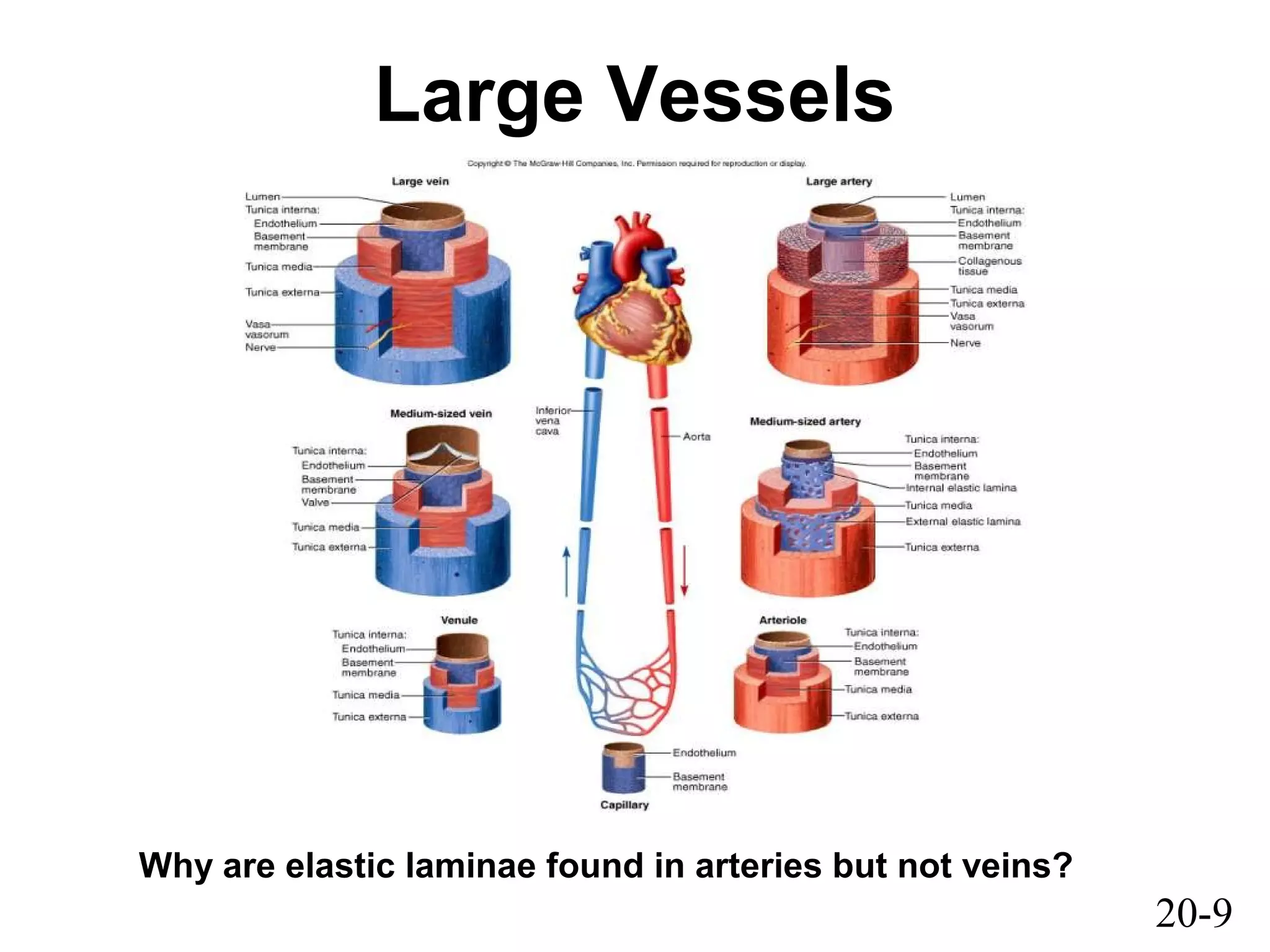
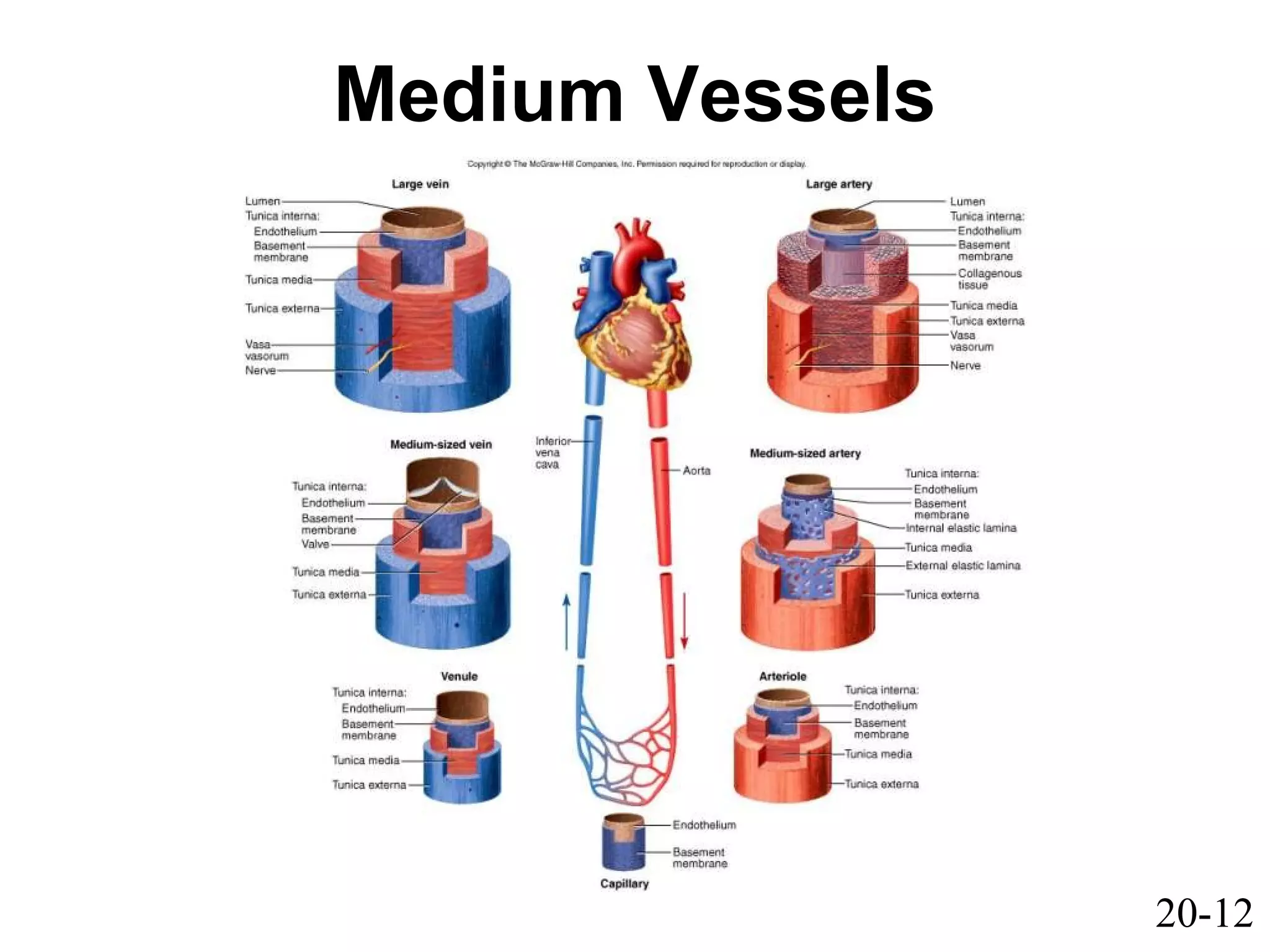
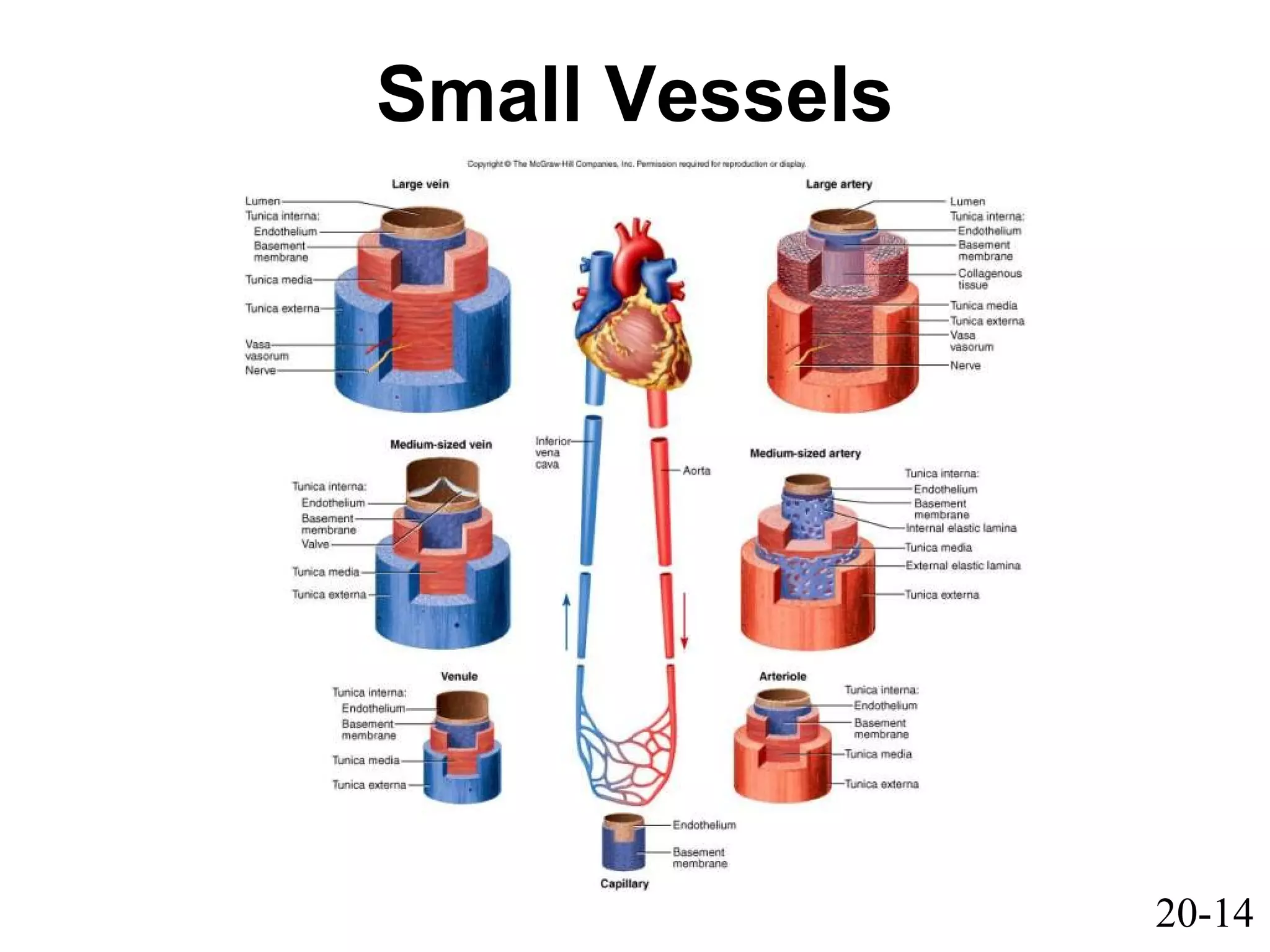
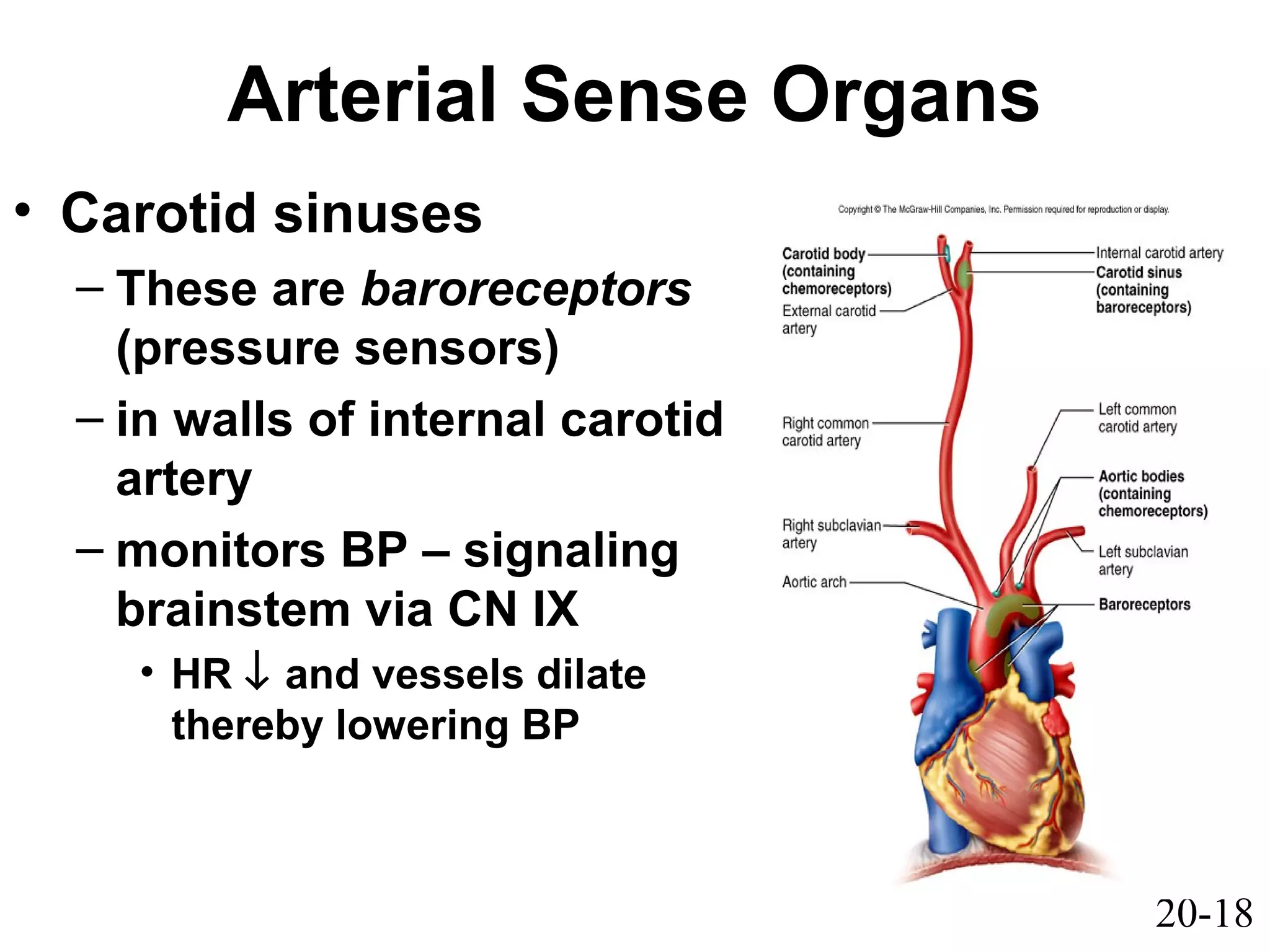
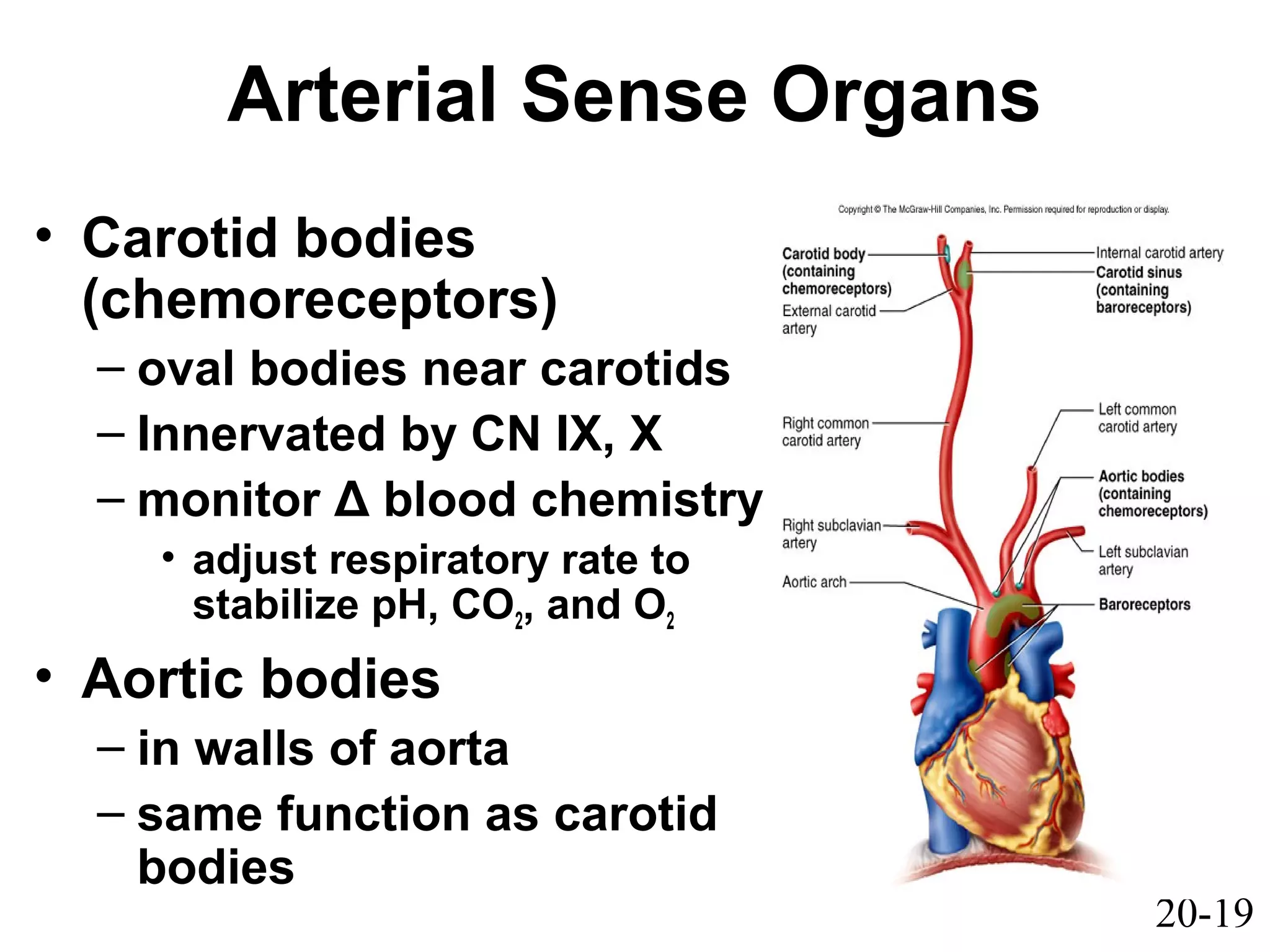
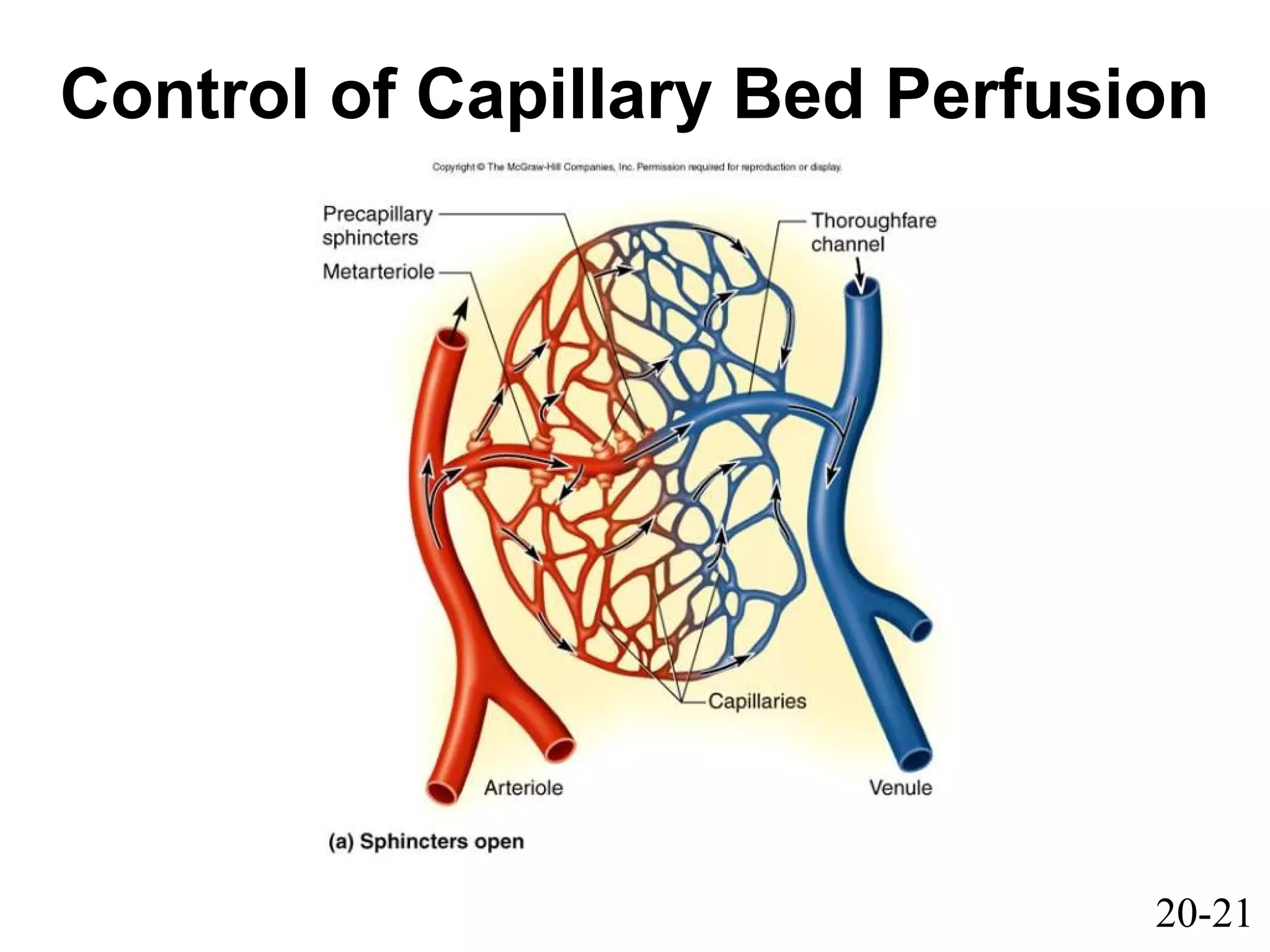
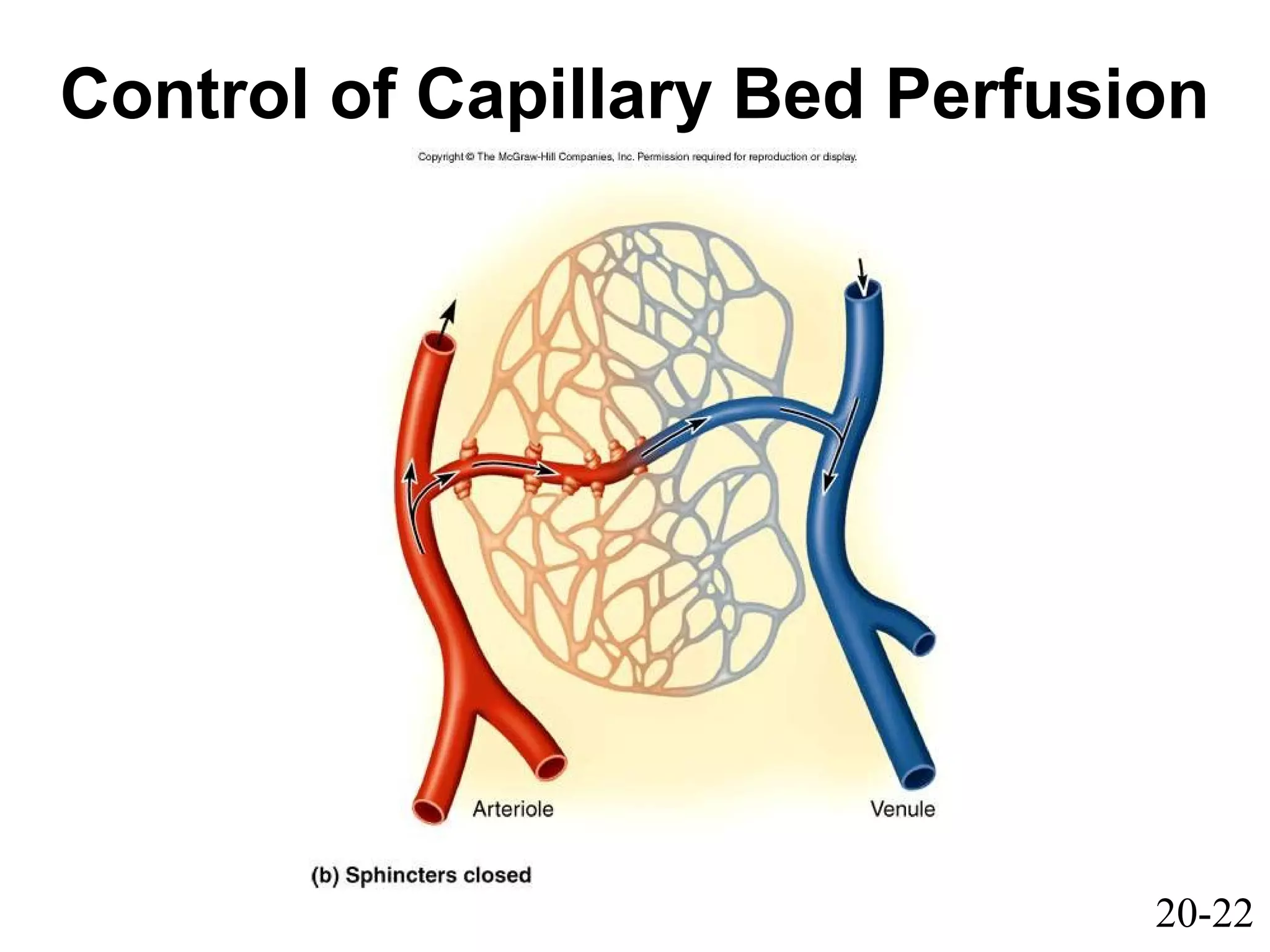
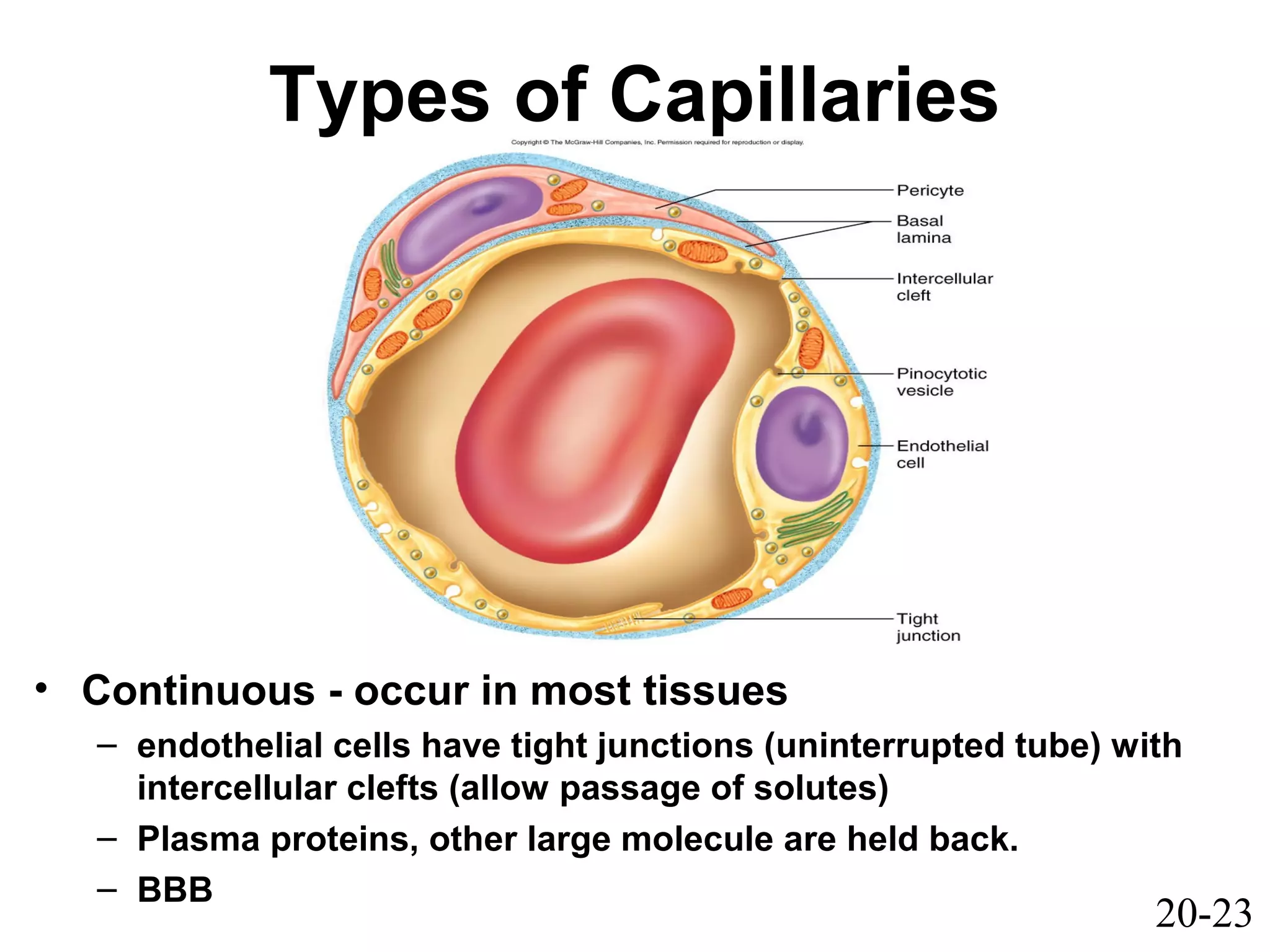
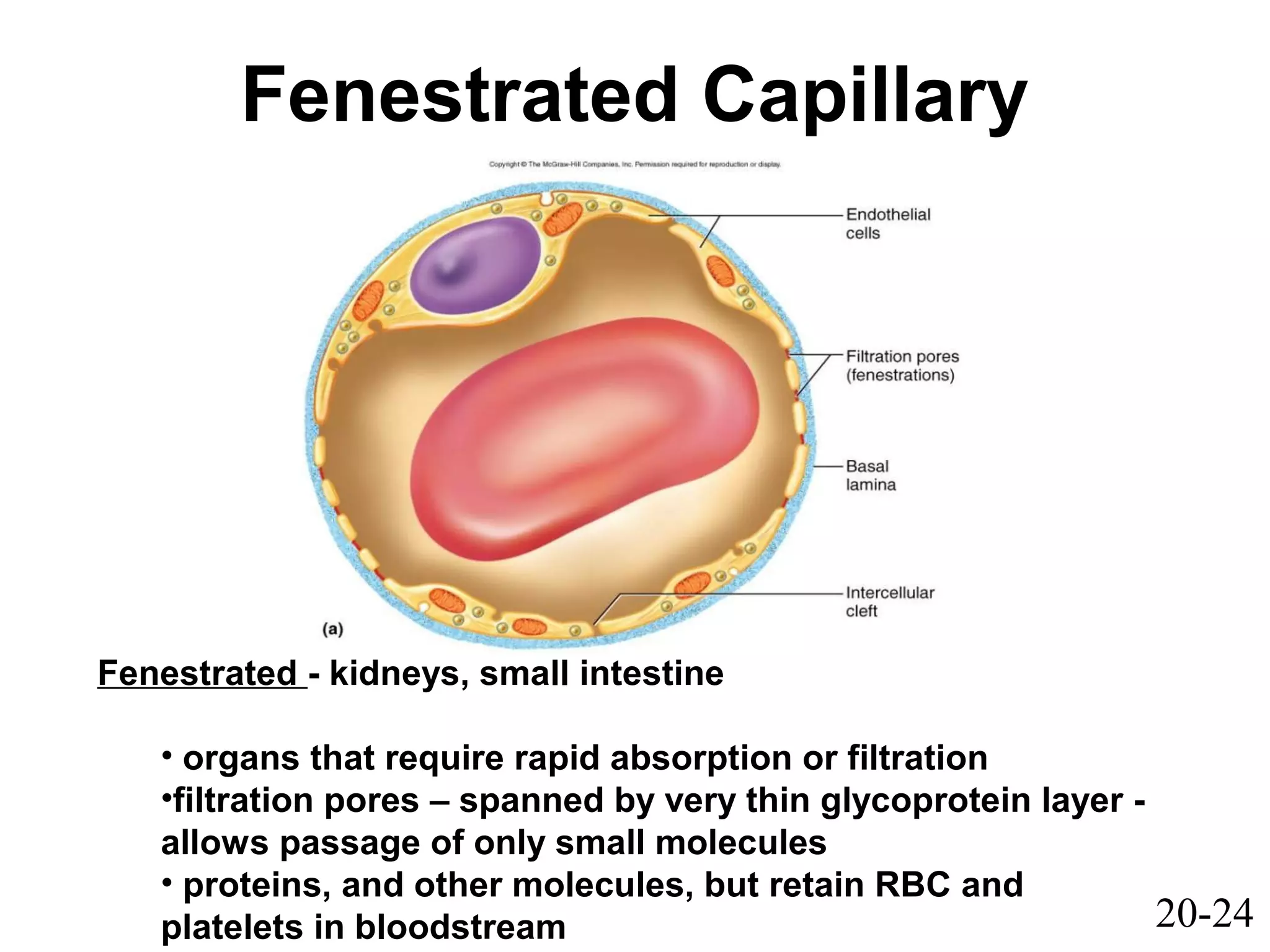
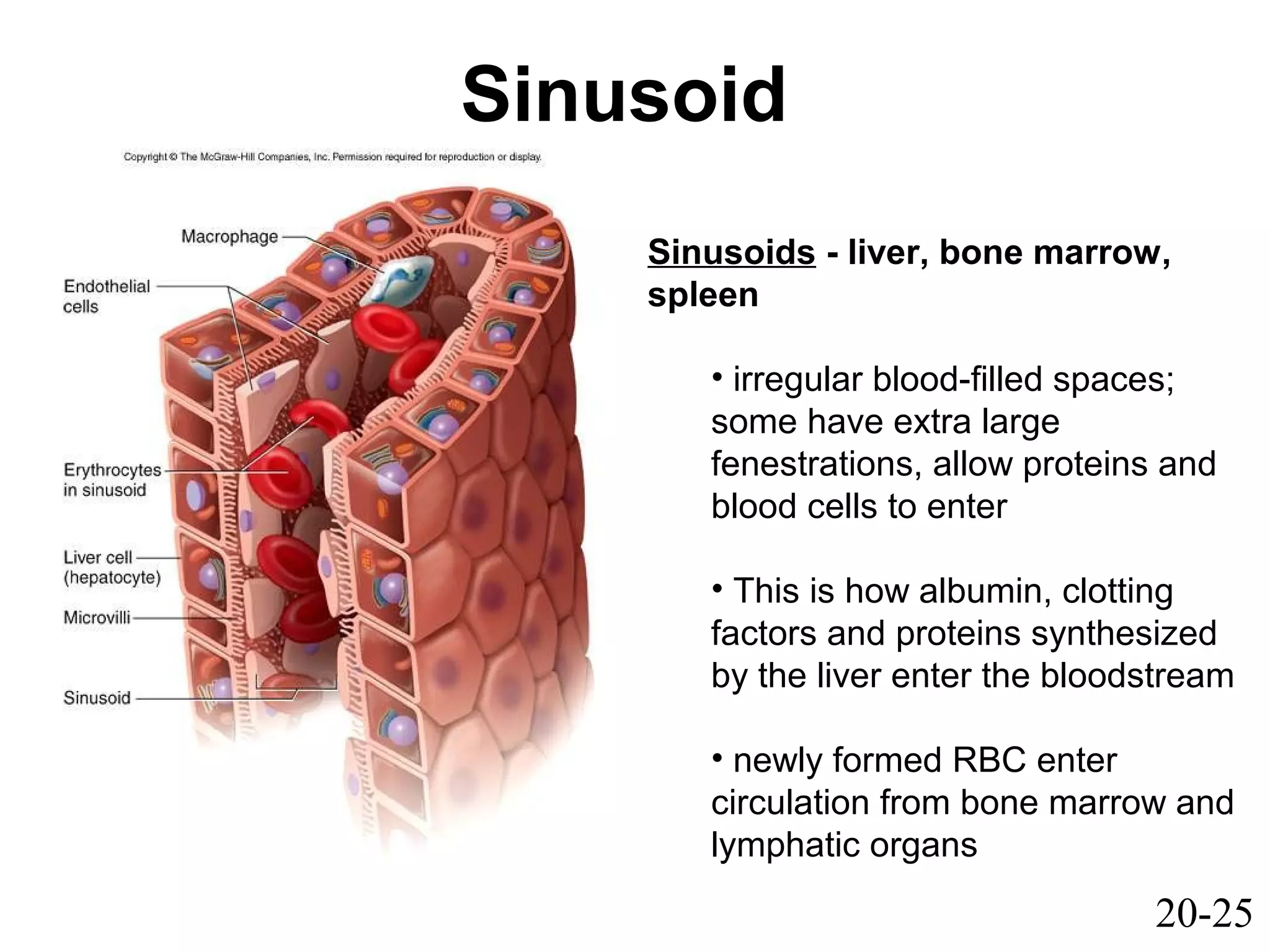
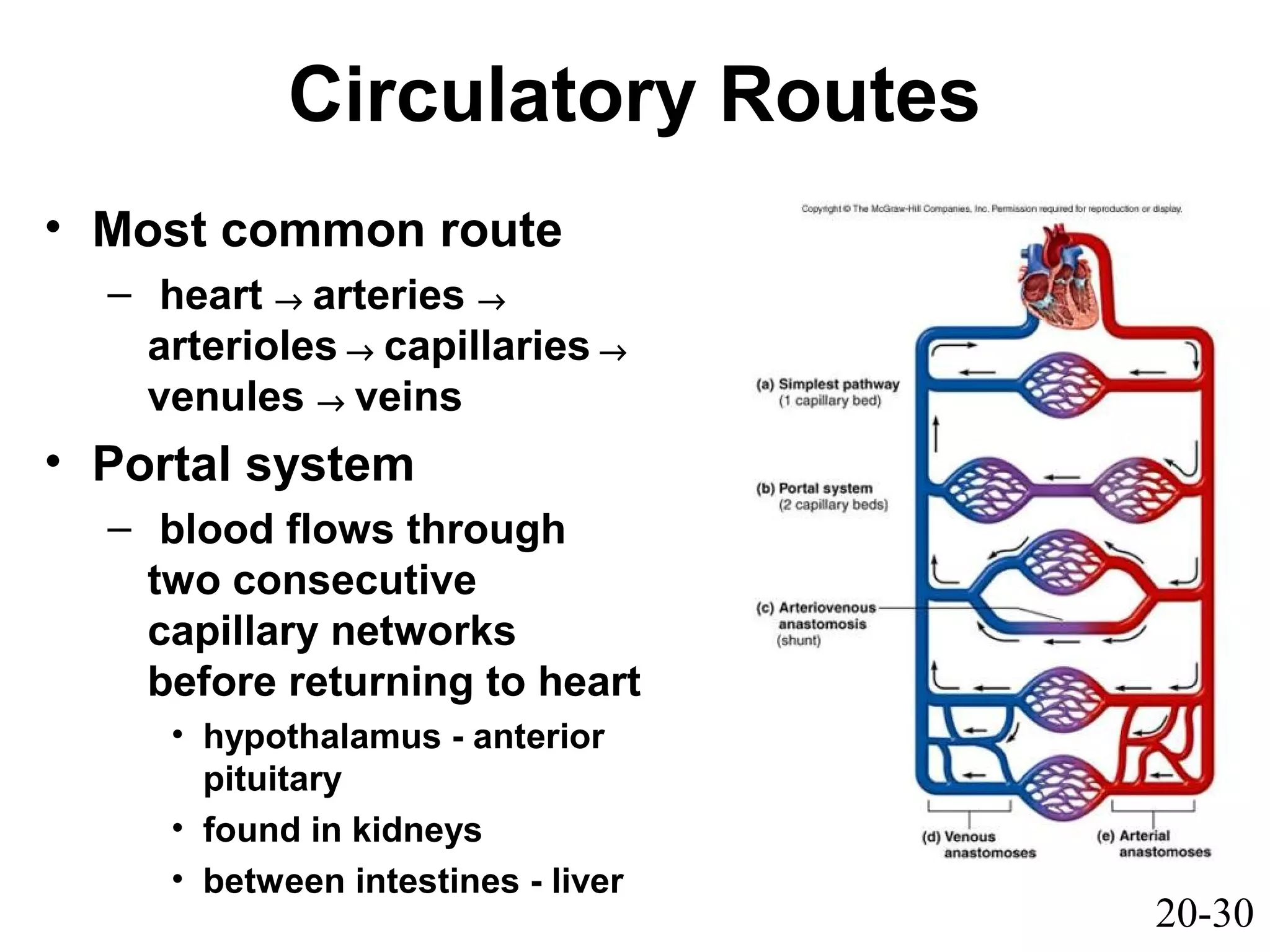
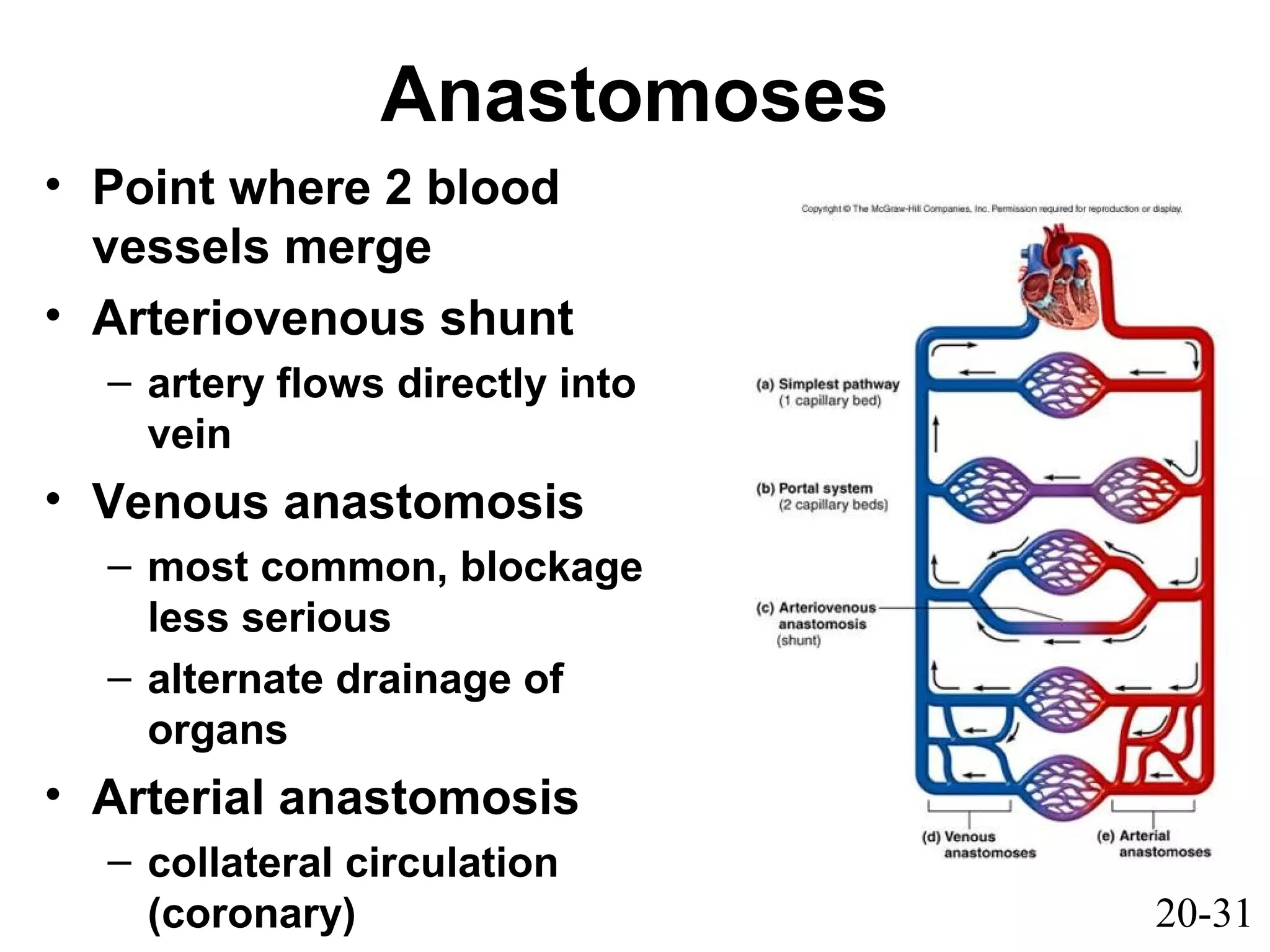
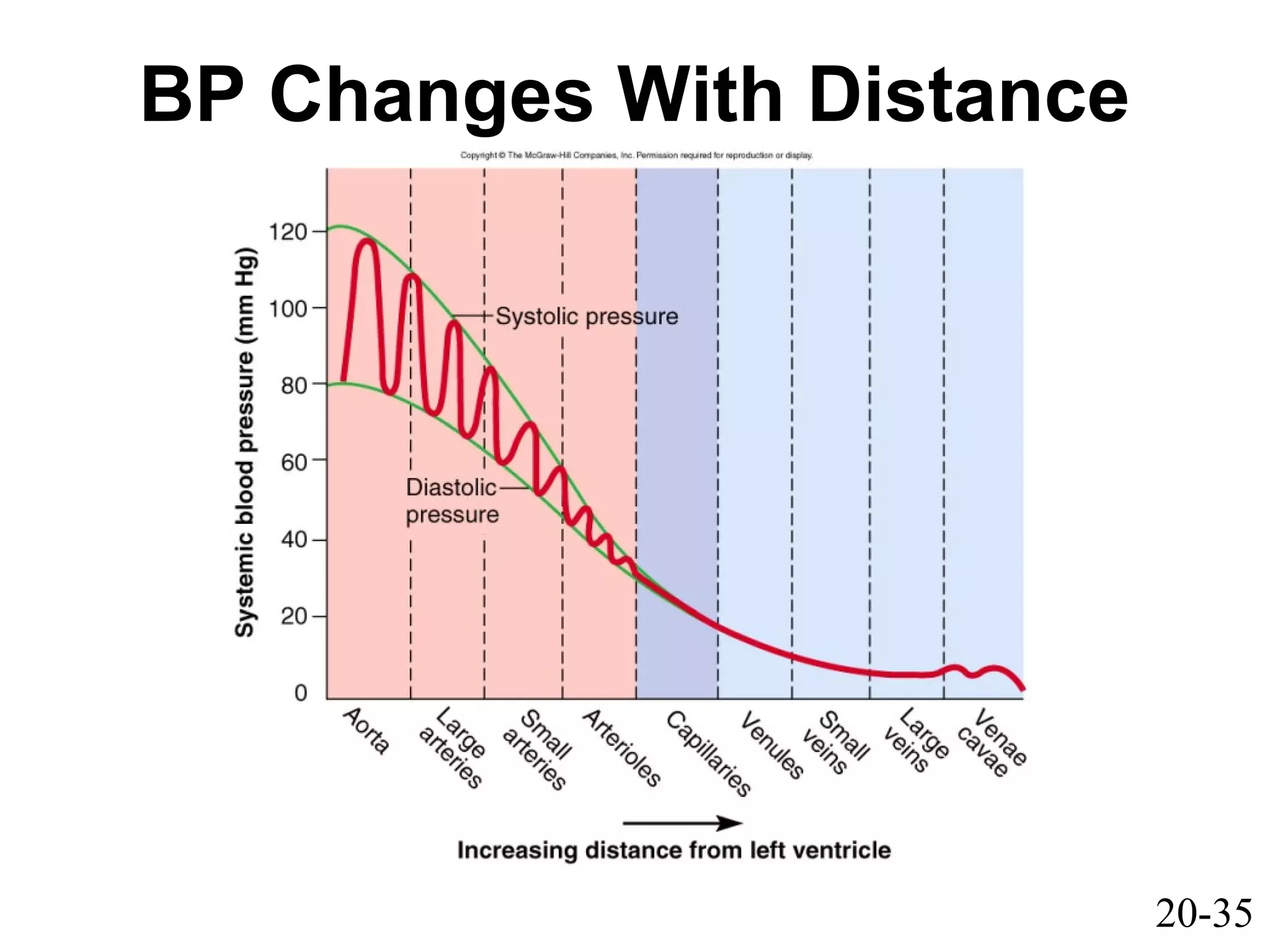
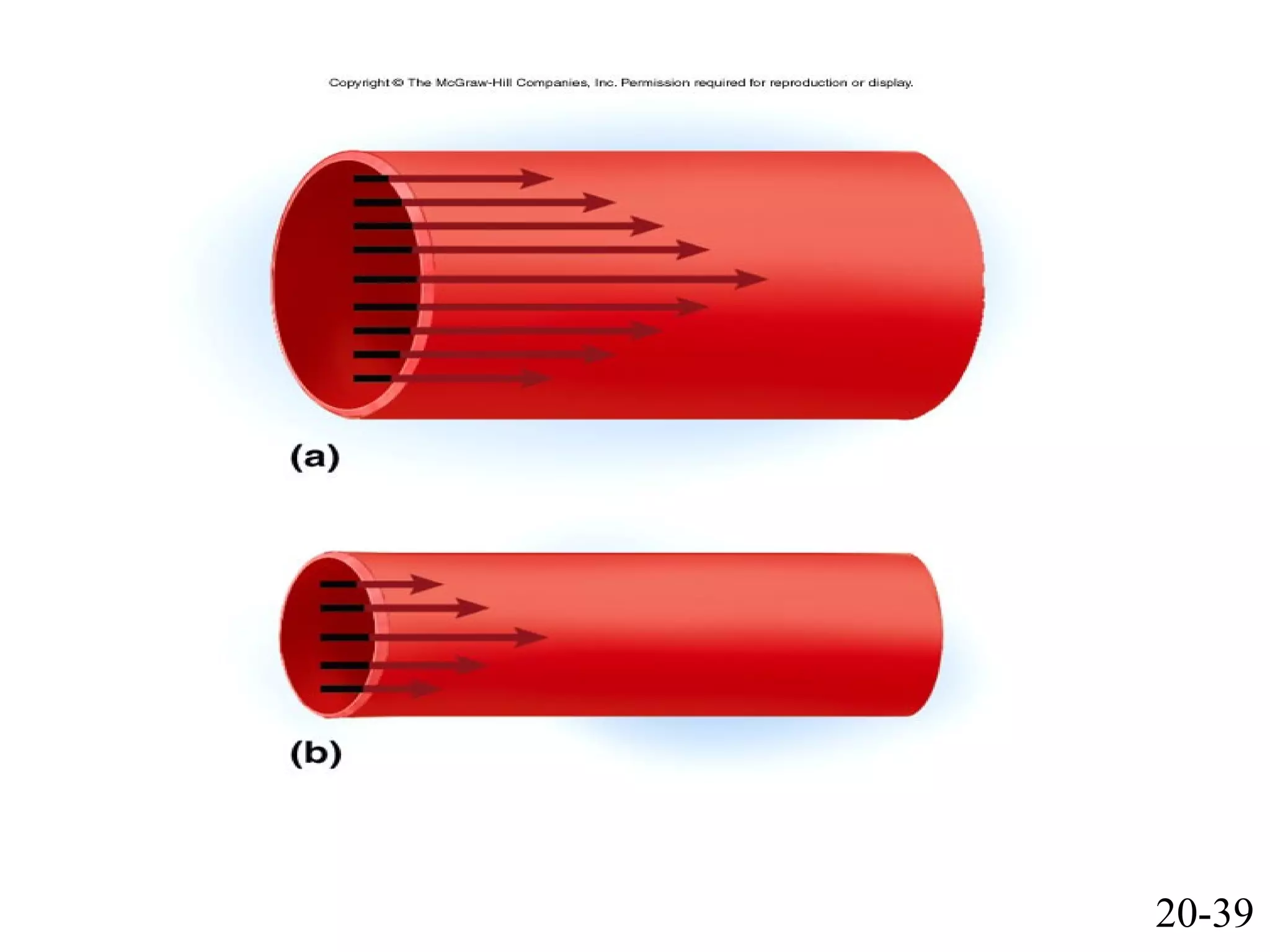
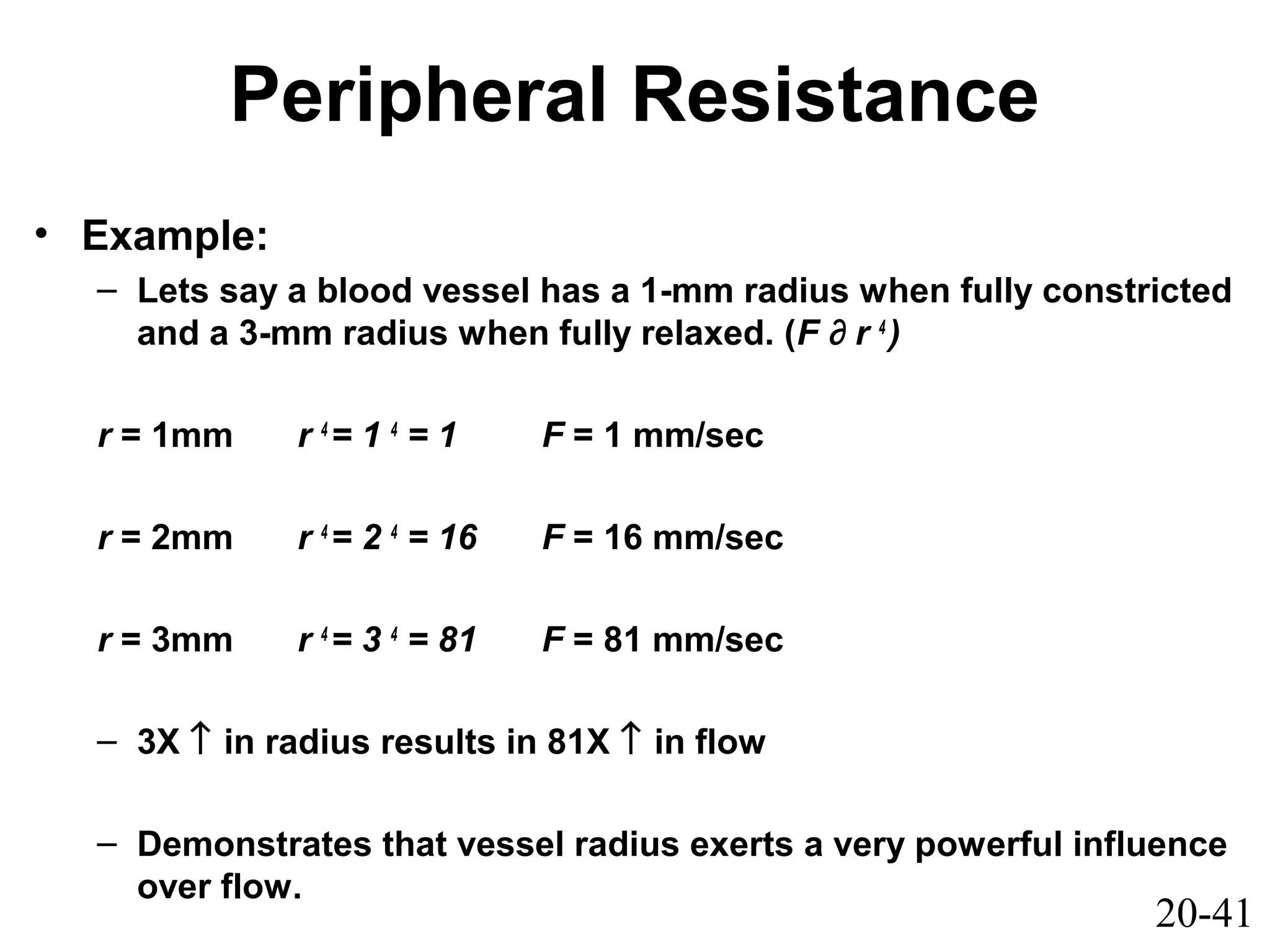
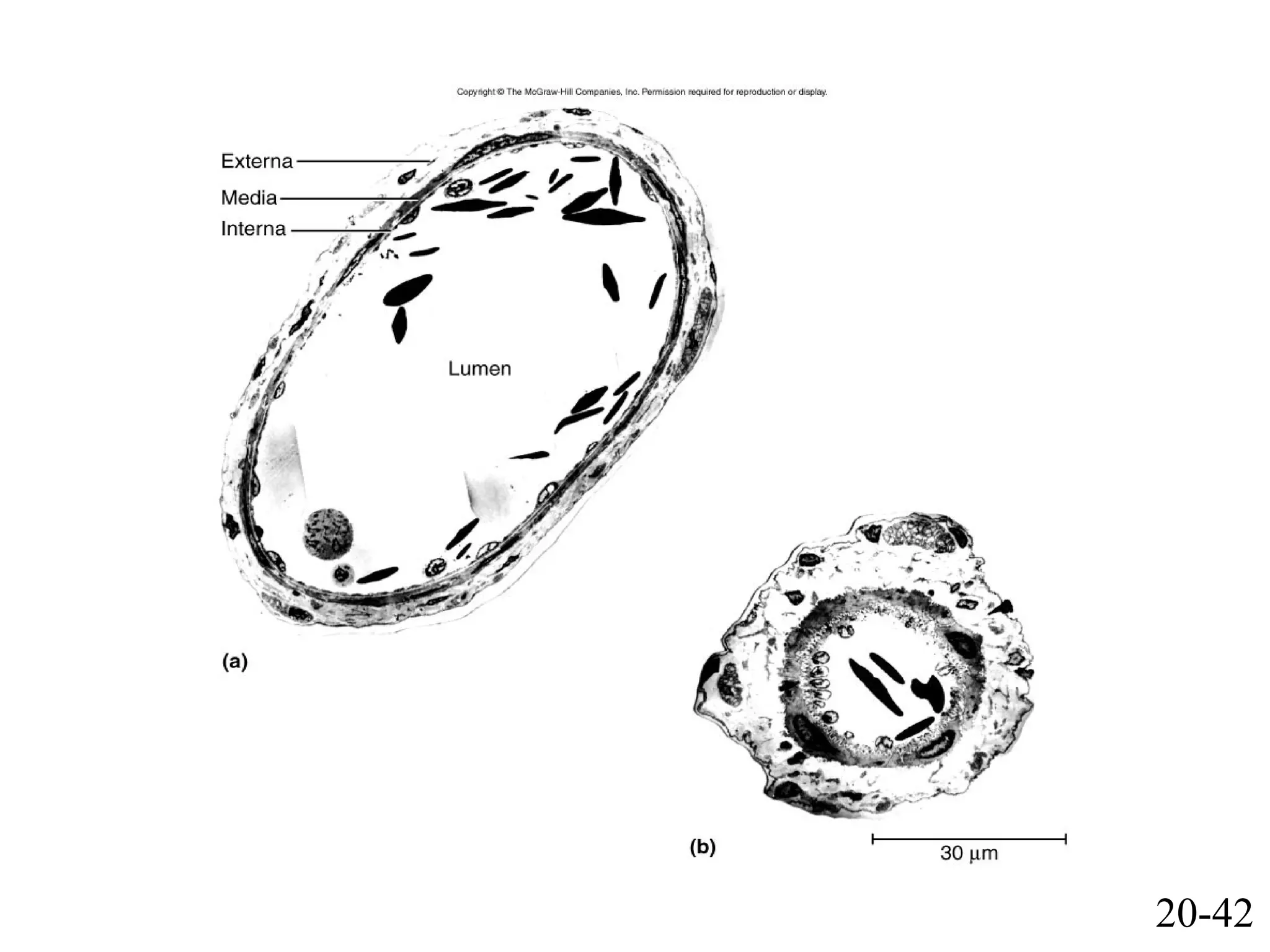
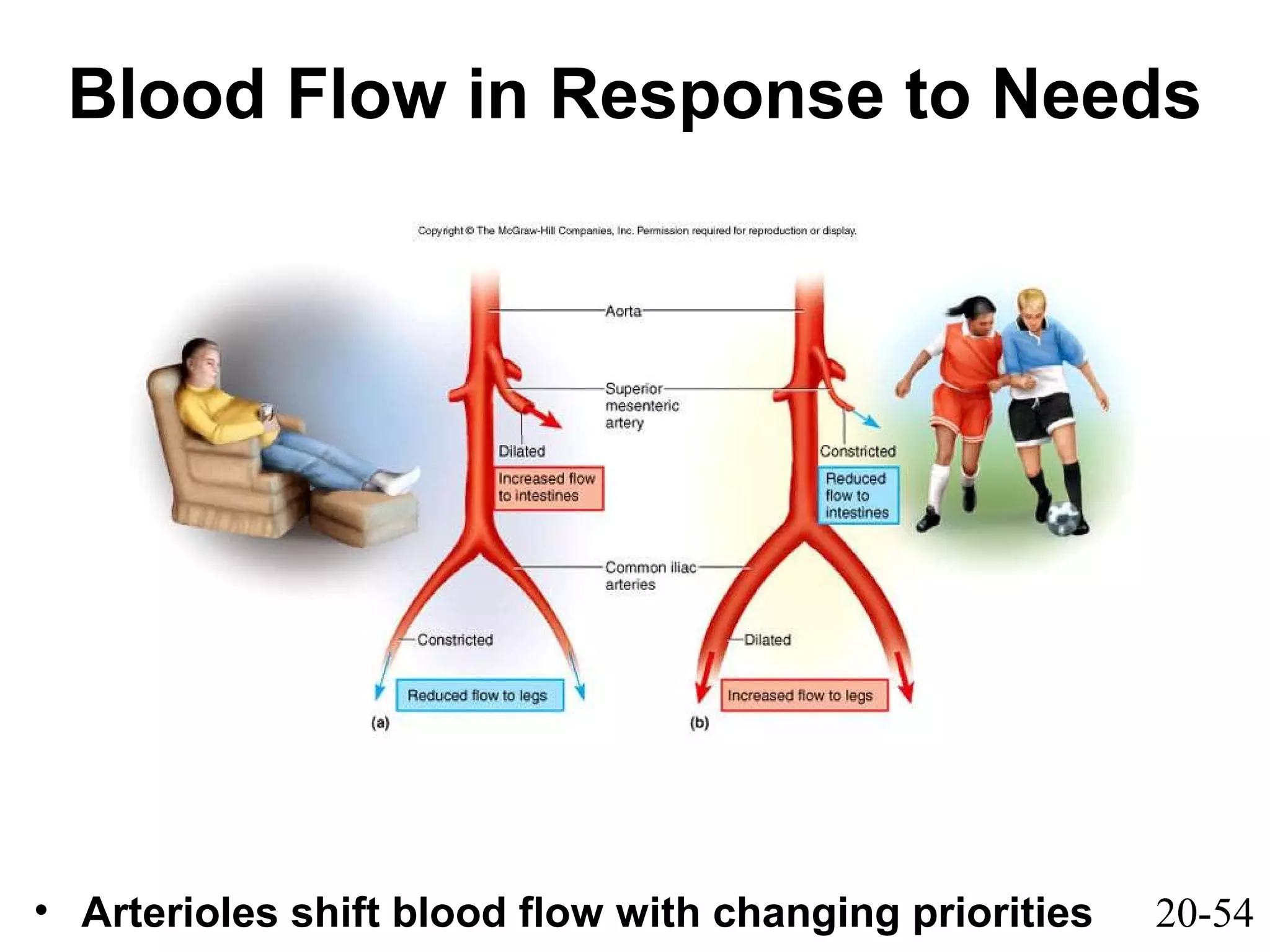
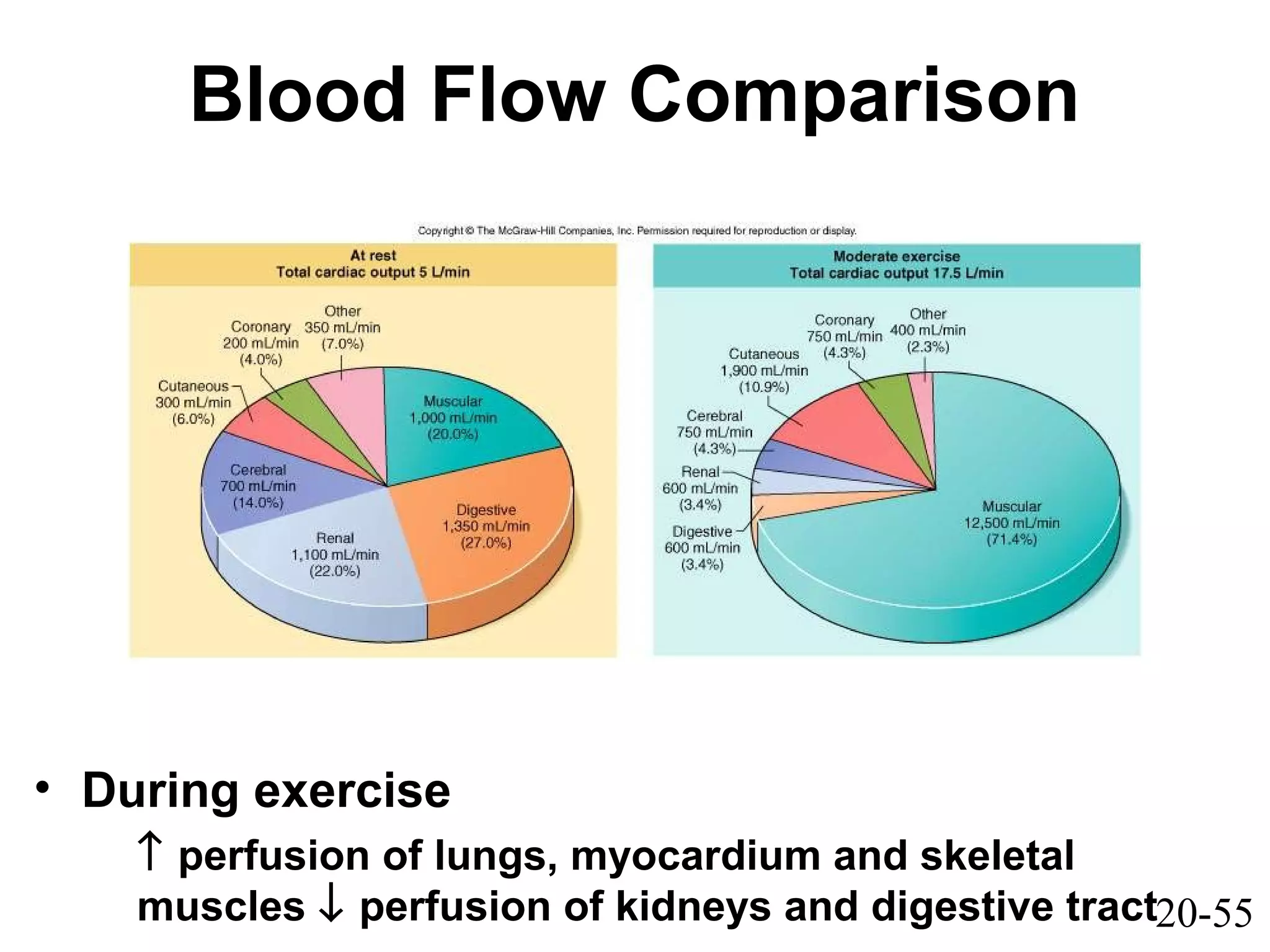
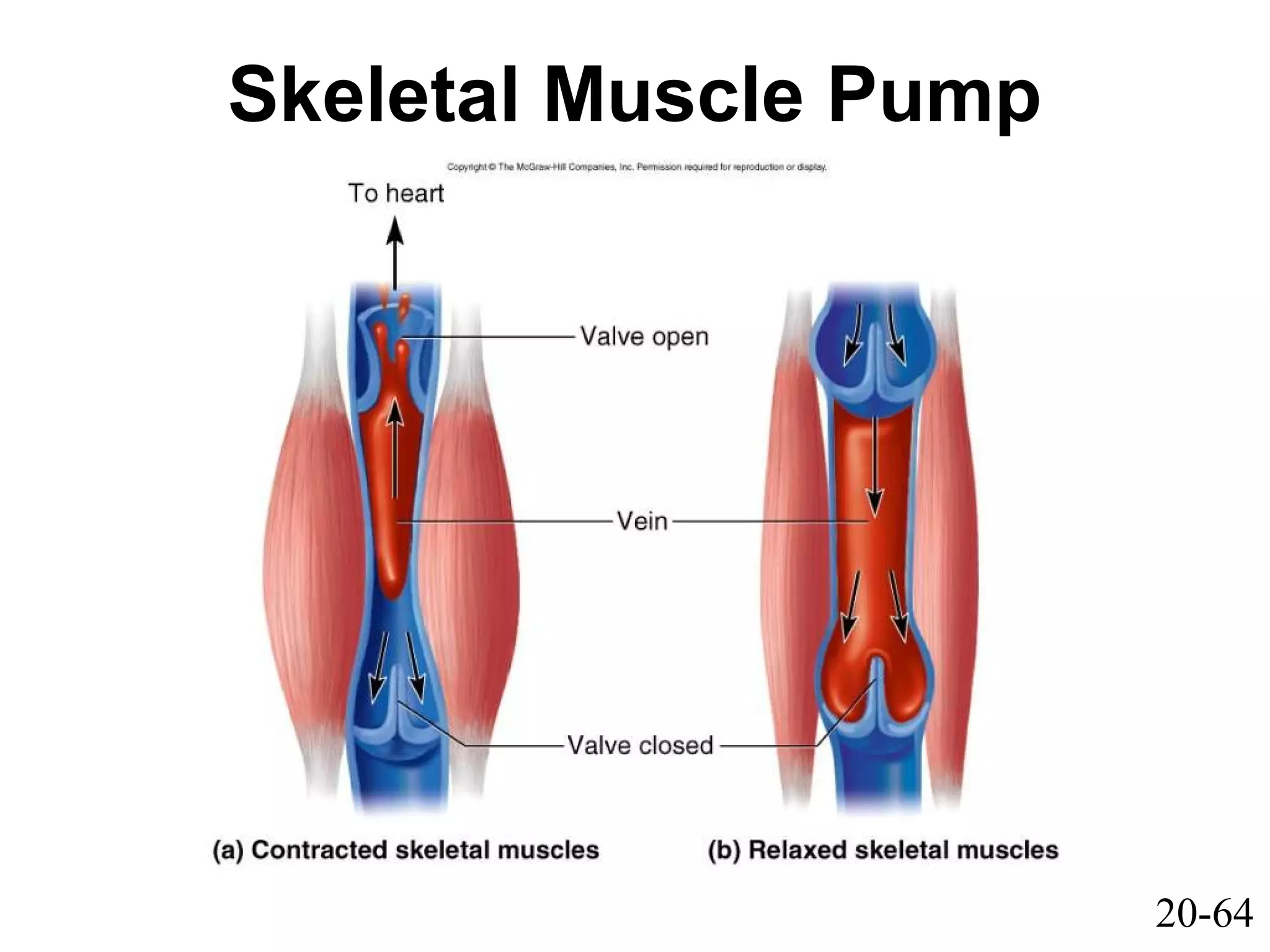
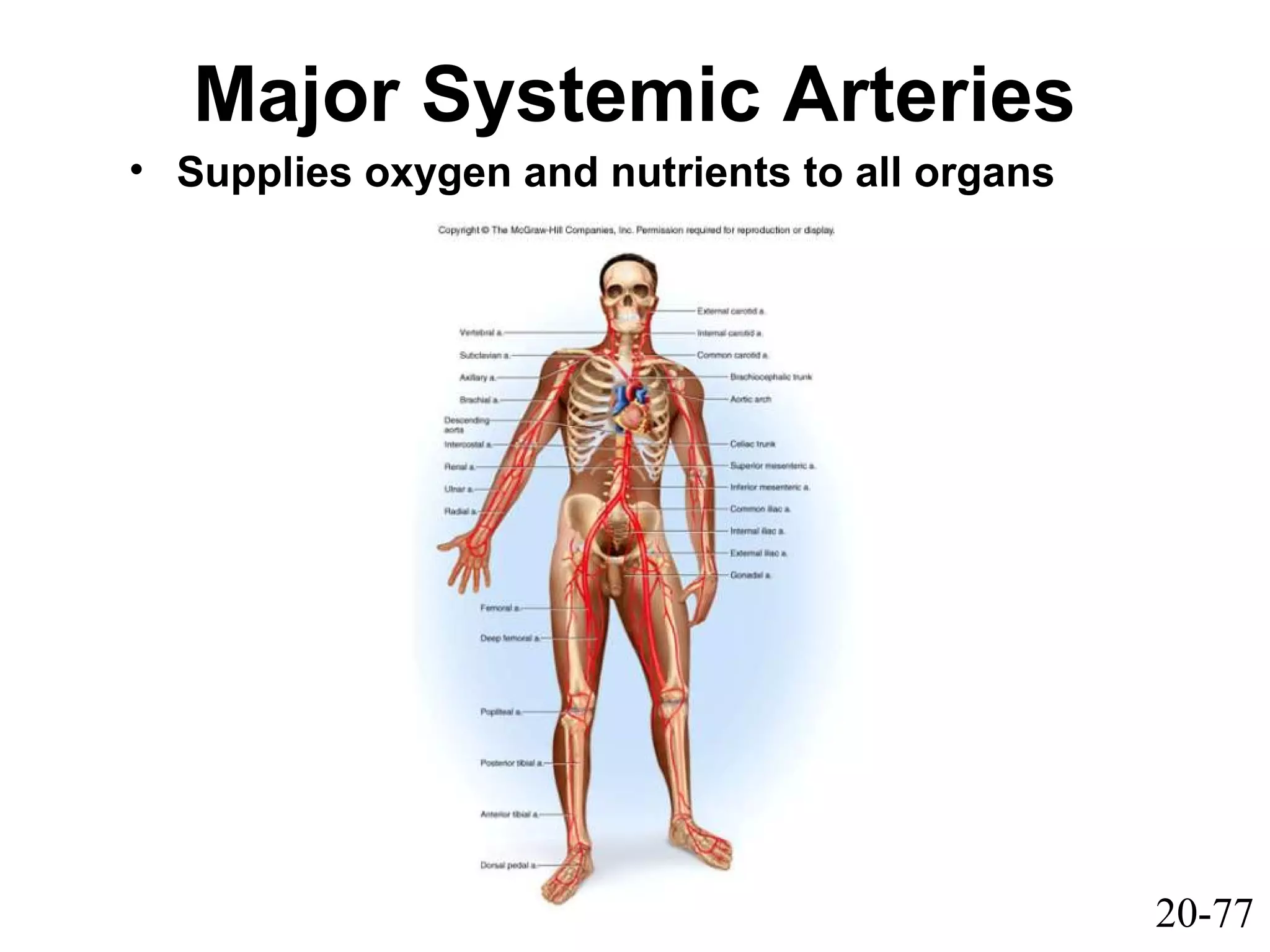
This document provides an overview of the circulatory system, including blood vessels and circulation. It describes the anatomy and layers of blood vessels, distinguishing between arteries, capillaries, and veins. Arteries are divided based on size into conducting, distributing, and resistance arteries. The roles of elastic tissue and smooth muscle in blood vessel walls are explained. Capillary types and their selective permeability is covered. Control of blood flow and factors influencing blood pressure such as resistance are summarized.