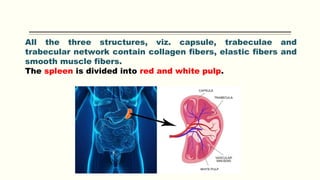
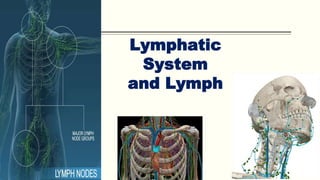
The reticuloendothelial system is a network of phagocytic cells that plays an important role in the body's defense mechanism. It includes reticuloendothelial cells found in the endothelial lining of blood vessels and lymph channels, as well as in connective tissue, organs like the spleen, liver, lungs and bone marrow. These cells are classified as either fixed tissue macrophages or wandering cells. Tissue macrophages carry out phagocytosis and secretion of various substances. The reticuloendothelial system aids immune function through phagocytosis, secretion of bactericidal agents, and secretion of cytokines.