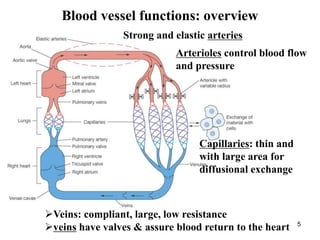
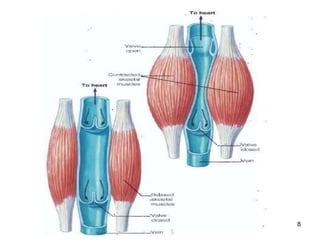
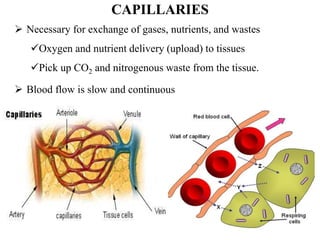
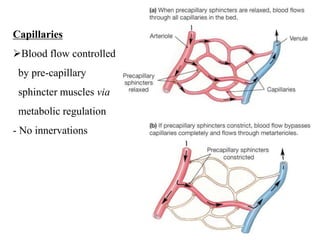
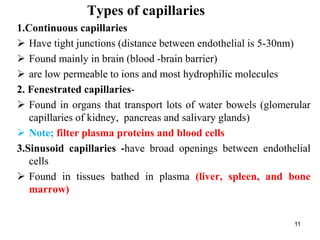
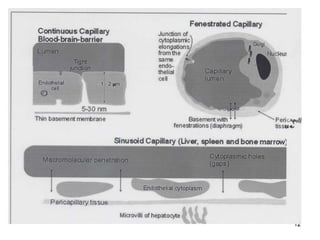
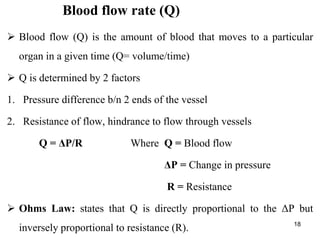
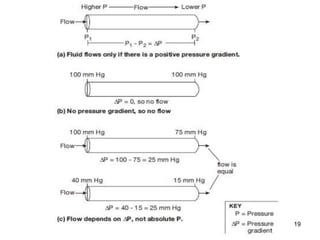
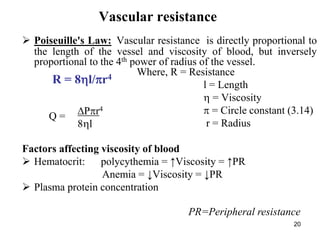
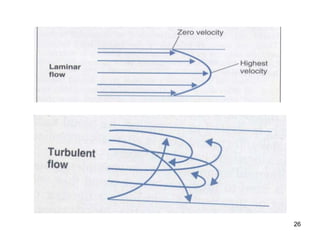
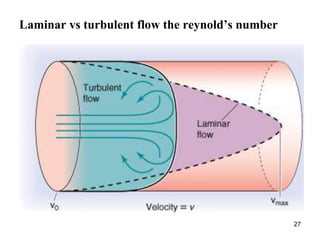
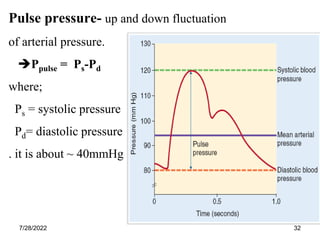
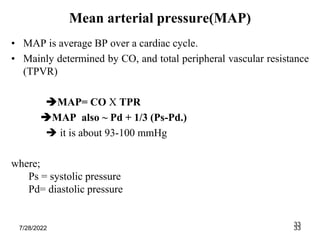
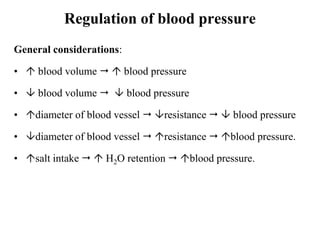
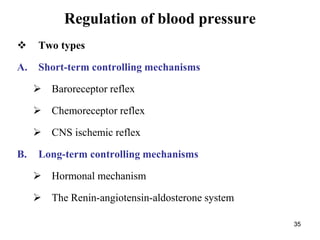
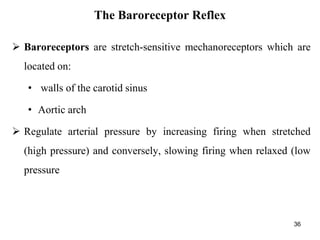
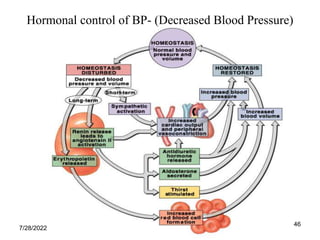
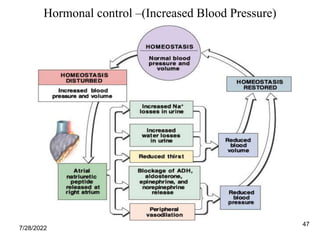
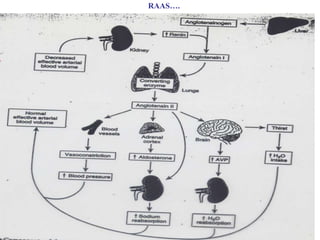
Hemodynamics is the study of blood flow, pressure, and resistance in the circulatory system. It includes the types and functions of blood vessels like arteries, veins, and capillaries. Arteries have thick elastic walls to withstand high blood pressure and distribute blood to tissues. Veins have thinner walls and valves to return blood to the heart. Capillaries allow for gas and nutrient exchange. Blood flow and pressure are regulated intrinsically through the vessels and extrinsically by the autonomic nervous and endocrine systems to meet the demands of tissues. The kidneys also help control blood volume and pressure long-term through the renin-angiotensin-aldosterone system.