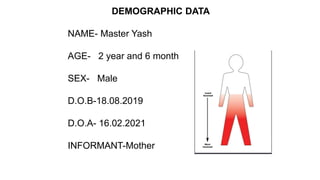
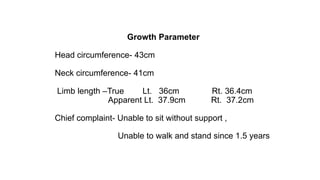
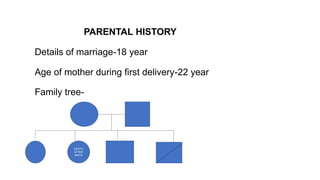
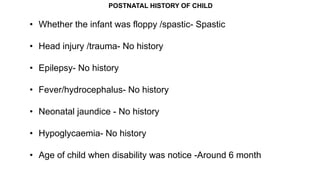
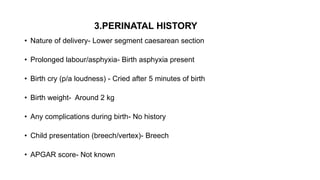
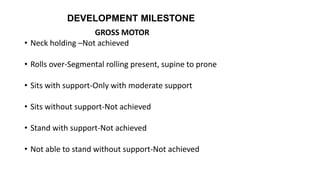
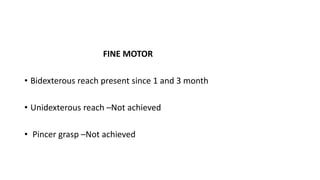
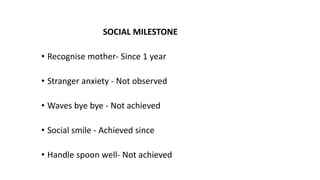
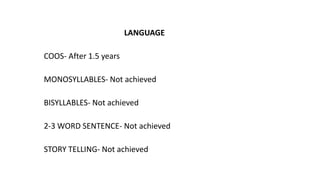
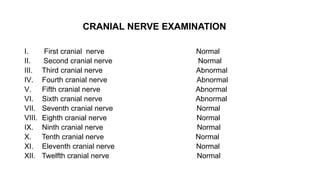
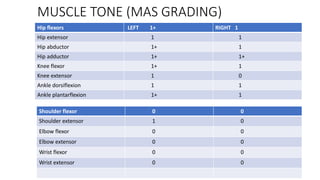
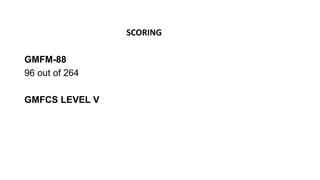
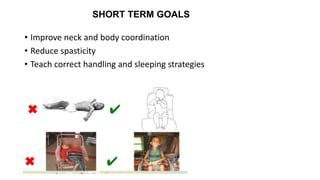
This document presents a case study of a 2 year and 6 month old male child diagnosed with cerebral palsy. It summarizes his medical history, developmental milestones, physical examination findings, and proposed treatment plan. The child exhibits delays in gross and fine motor skills and language development. He is unable to sit, stand or walk independently. The treatment plan focuses on stretching tight muscles, improving range of motion, strengthening, and working on functional activities like sitting, standing and mobility with the long term goals of independent ambulation and self-care.