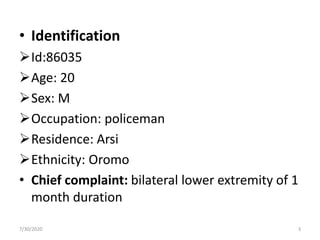
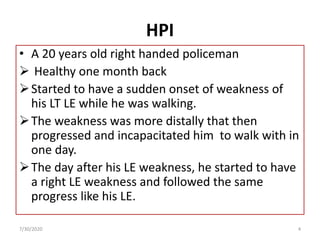
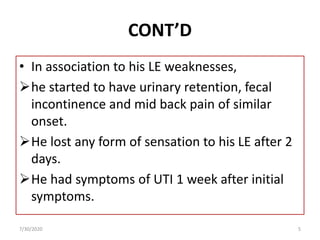
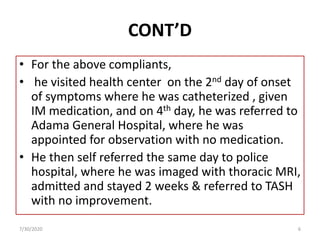
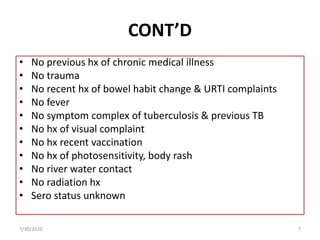
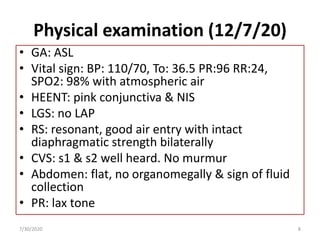
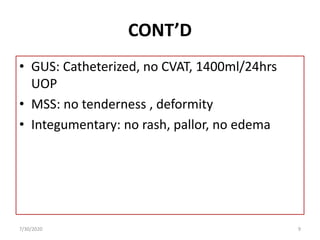
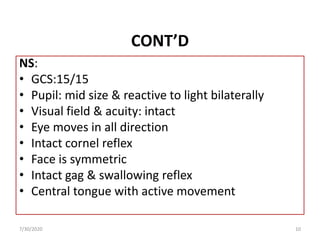
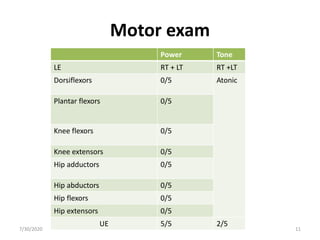
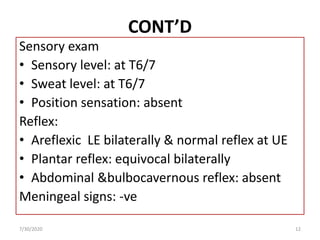
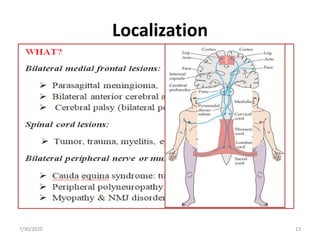
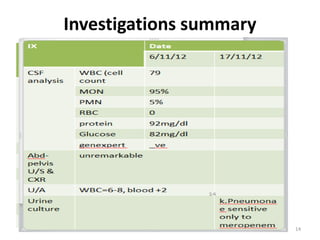
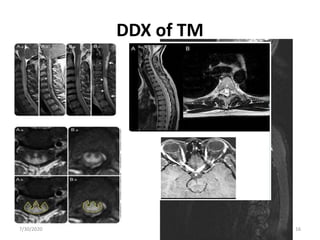
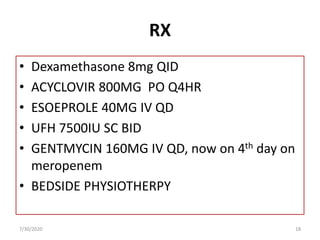
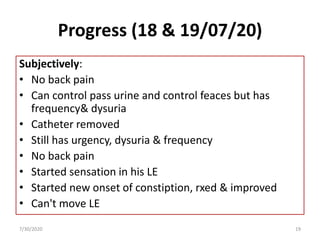
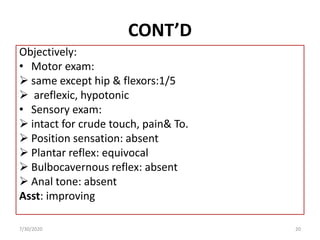
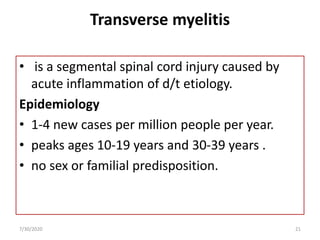
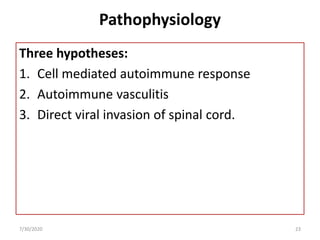
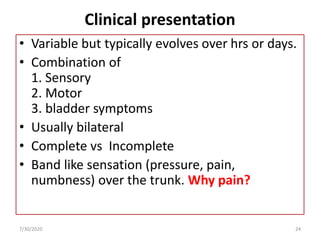
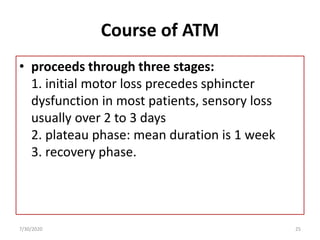
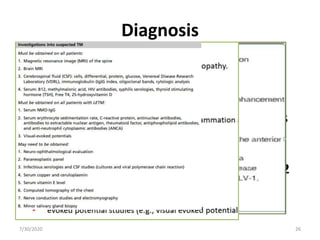
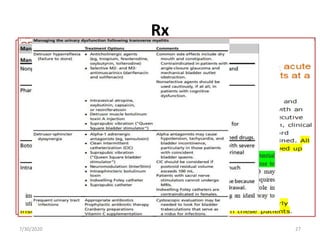
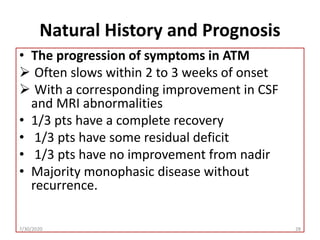
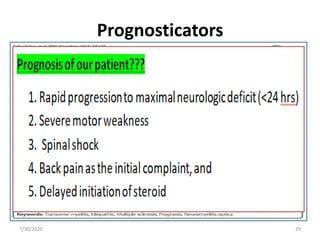
This document presents a case study of a 20-year-old male patient diagnosed with Transverse Myelitis (TM). The patient presented with sudden bilateral lower extremity weakness and loss of sensation that progressed over one month. Investigations including MRI and CSF analysis confirmed the diagnosis of TM. The patient was treated with high-dose steroids, antivirals, antibiotics, and physiotherapy. His symptoms showed signs of gradual improvement over time. The document also provides background information on TM, including causes, pathophysiology, clinical presentation, diagnosis, treatment options and prognosis.