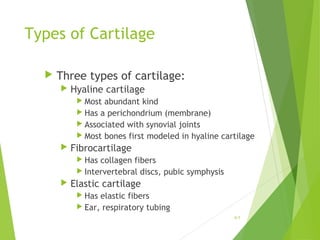
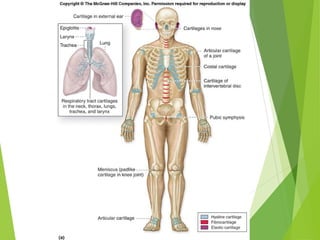
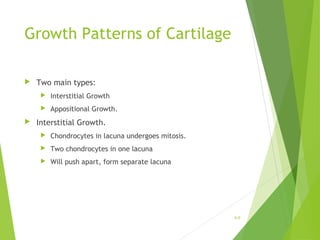
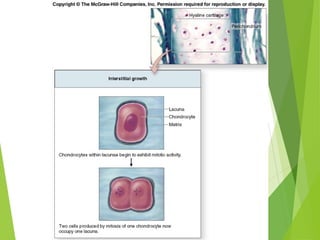
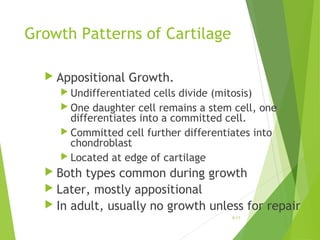
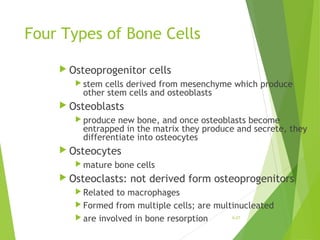
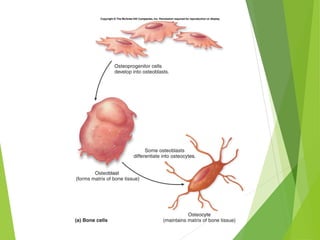
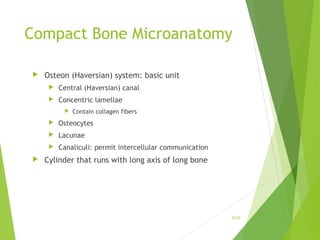
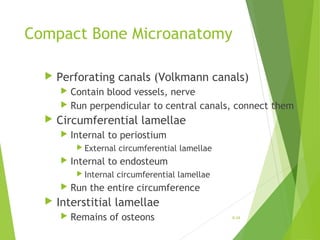
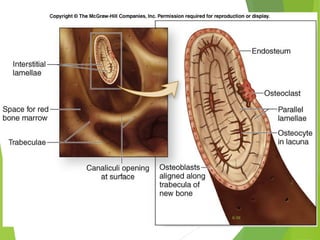
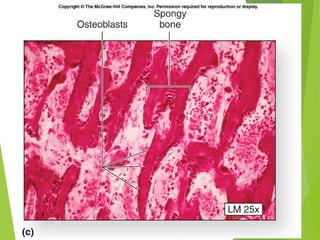
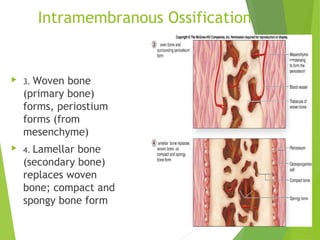
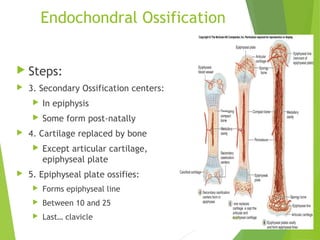
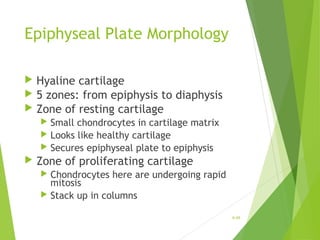
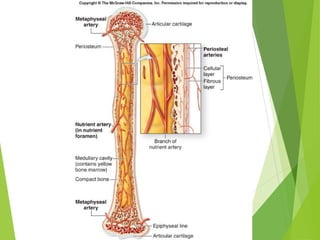
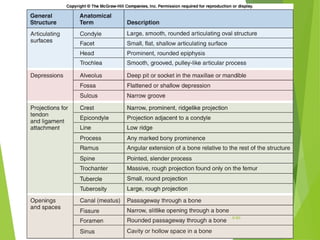
This document discusses the skeletal system and its components. It covers the definitions of osteology, arthrology, and the types of cartilage. It describes the functions of the skeletal system which include support, protection, movement, blood cell formation, mineral storage, and serving as an energy reserve. The document outlines the structures of long bones and flat bones. It explains the processes of ossification, including intramembranous ossification and endochondral ossification. In addition, it covers bone cells, bone growth and remodeling, blood supply, and the effects of hormones on bone.