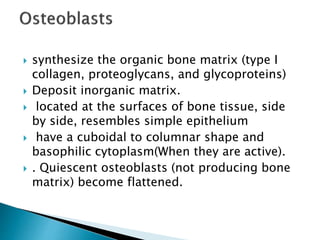
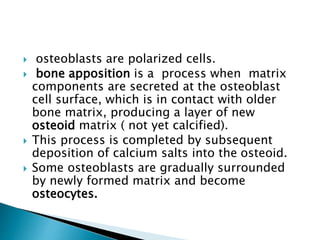
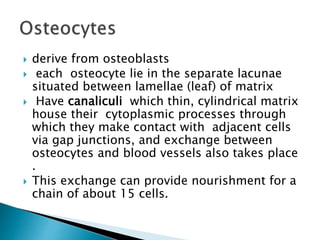
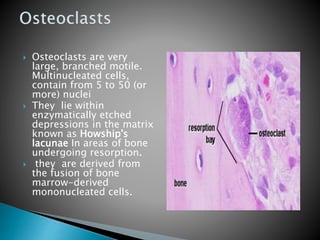
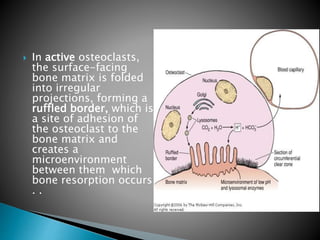
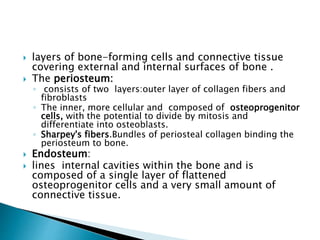
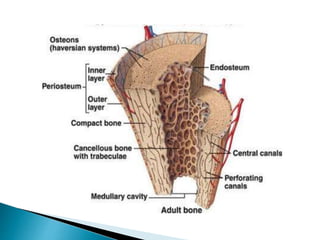
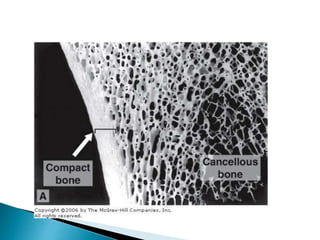
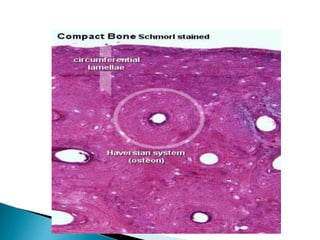
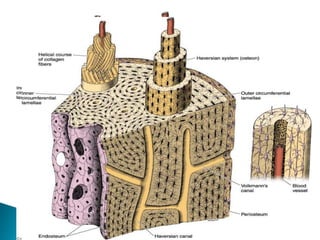
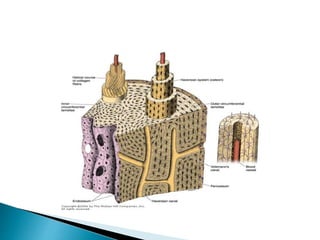
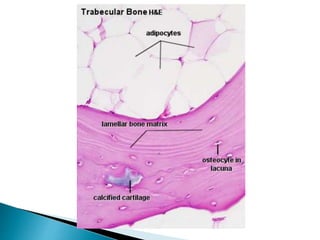
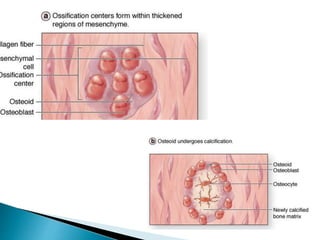
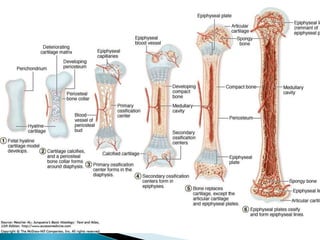
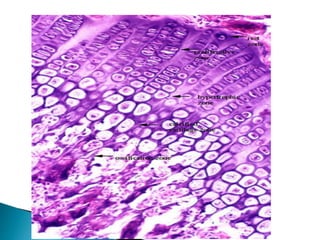
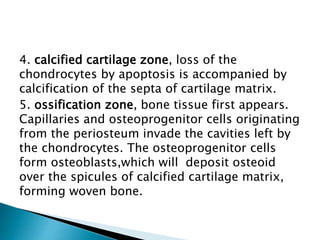
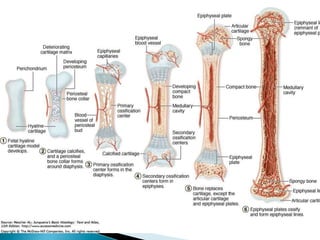
The document discusses the structure and function of bone tissue, emphasizing its composition, types of cells, and the processes of ossification. It explains the roles of osteoblasts, osteocytes, and osteoclasts in bone formation and maintenance, as well as the distinctions between compact and trabecular bone. Additionally, it outlines mechanisms of intramembranous and endochondral ossification, detailing the growth and development of bones during different life stages.