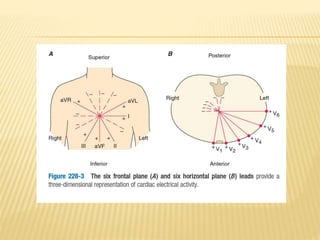
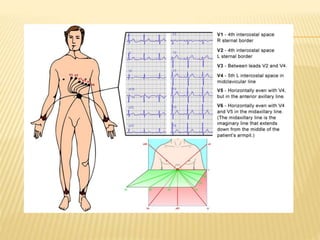
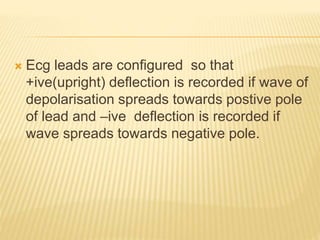
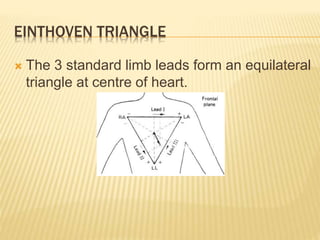
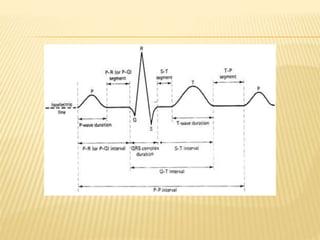
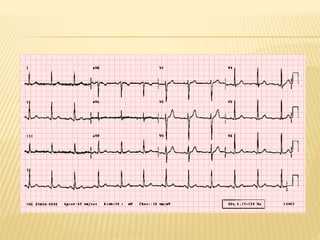
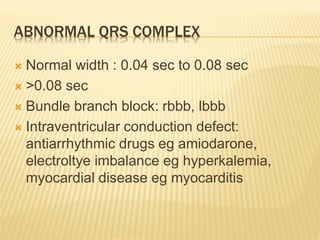
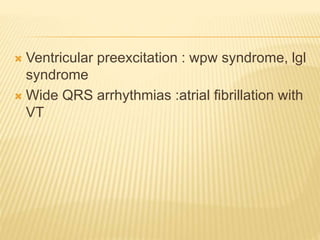
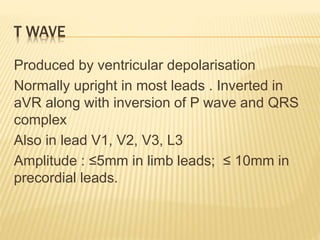
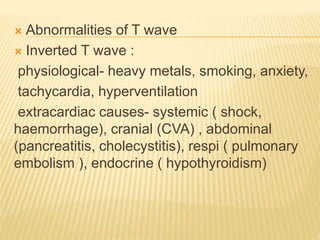
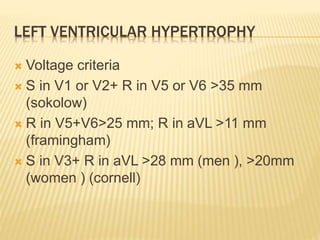
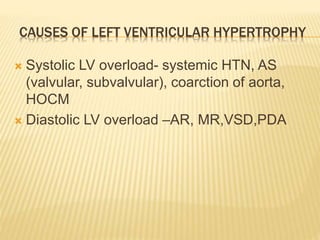
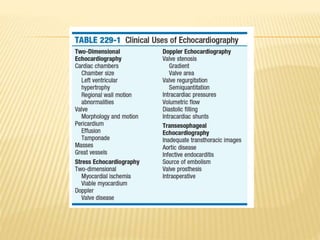
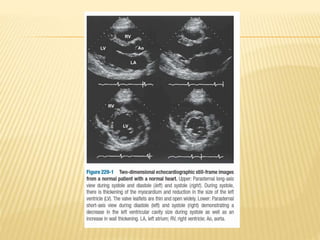
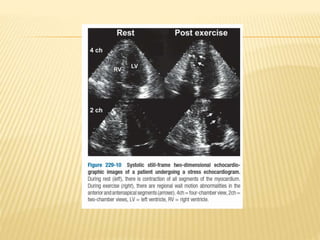
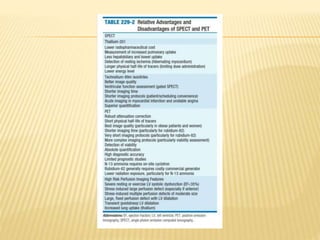
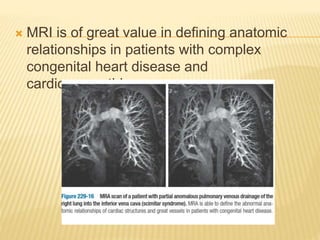
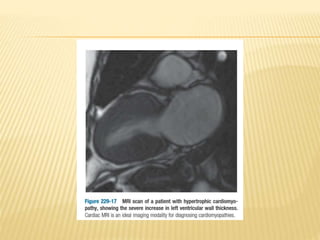
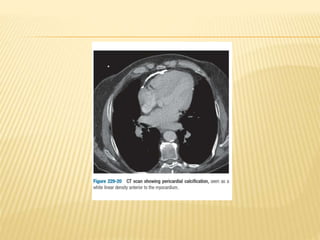
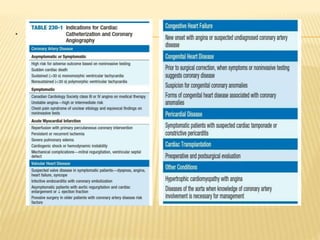
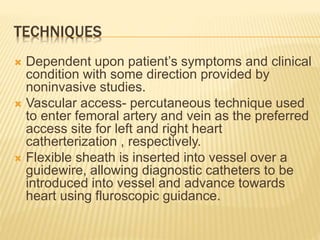
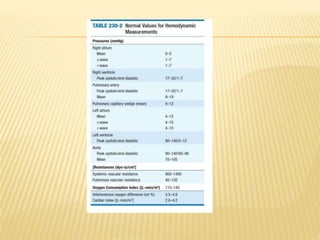
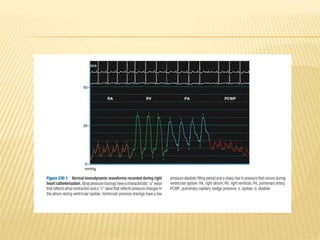
This document provides an overview of various diagnostic tools used in cardiology, including electrocardiography (ECG), non-invasive cardiac imaging modalities like echocardiography and nuclear imaging, and invasive diagnostic procedures like cardiac catheterization and coronary angiography. It describes the basic principles, clinical applications, and abnormalities detected by each diagnostic modality.