The document provides information on various cardiac diagnostic and laboratory tests including:
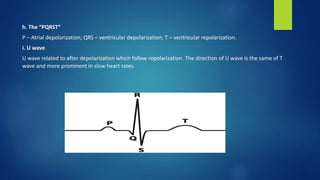
1. ECG - Analyzes electrical events of the cardiac cycle and can provide insight into pathophysiology. Important aspects to analyze include rhythm, intervals, axis, and waves.
2. Treadmill test - Progressive exercise test to evaluate cardiovascular response. Used to detect ischemia by analyzing ECG changes, symptoms, and hemodynamics.
3. Echocardiography - Ultrasound of the heart to assess structure, function, valves, and flow. Provides different views of the heart chambers and valves.
4. Holter monitoring - Mobile ECG recording over 24-72 hours to detect arrhythmias and ST-T changes