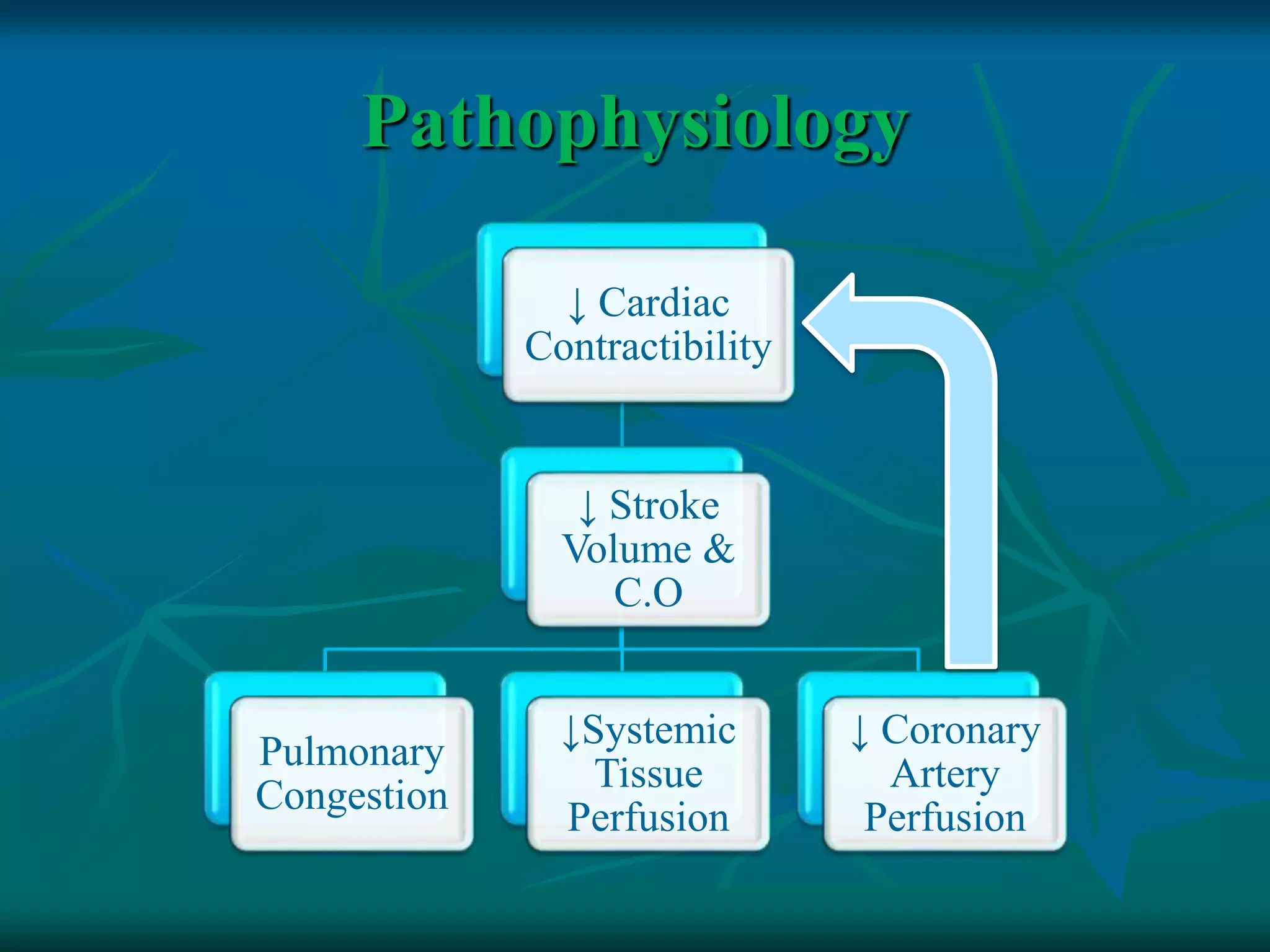
Cardiogenic shock is a condition resulting from the heart's inability to pump blood efficiently, often caused by severe heart attacks and associated with high mortality rates. Key factors include pre-existing heart conditions, hypertension, diabetes, and obesity, with clinical manifestations such as chest pain, diminished heart sounds, and low blood pressure. Management involves correcting underlying causes, pharmacological treatments, surgical options, and nursing care focused on monitoring and prevention strategies.