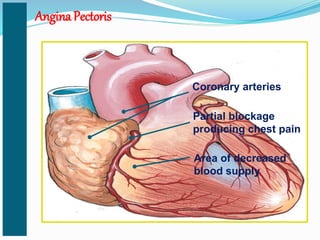
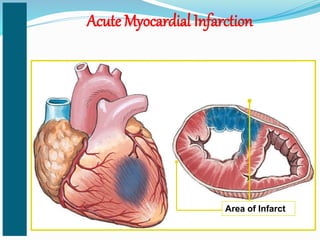
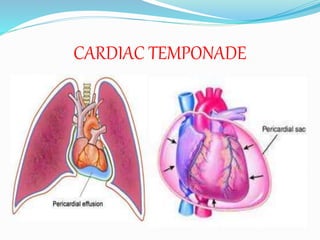
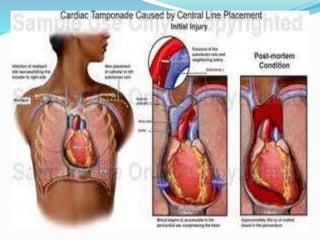
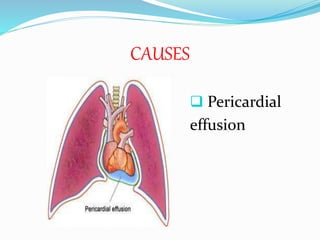
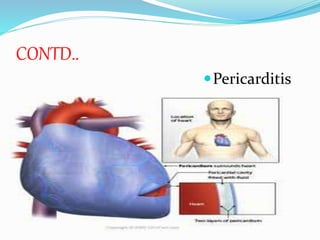
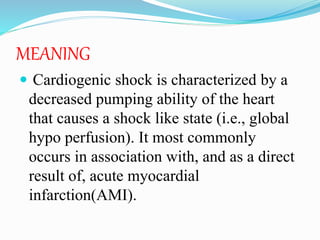
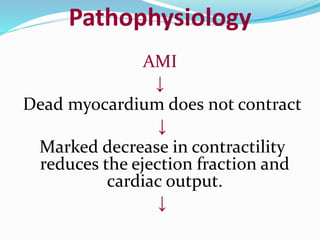
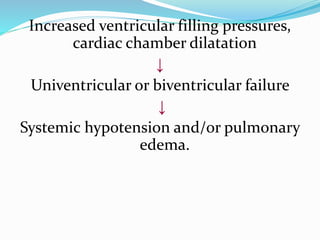
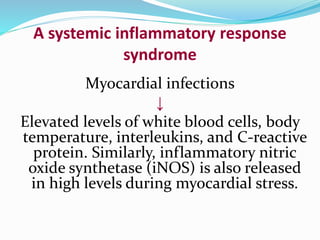
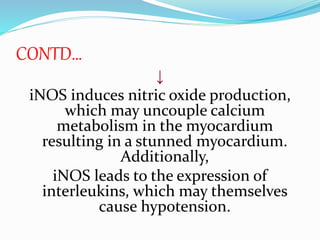
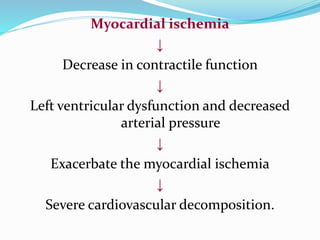
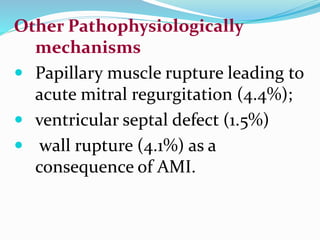
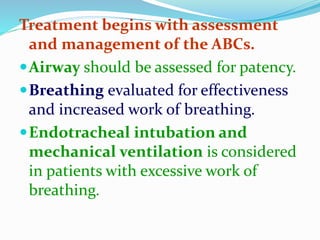
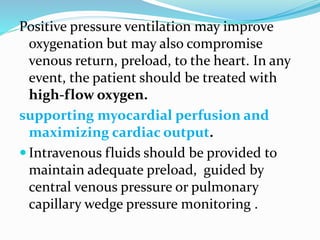
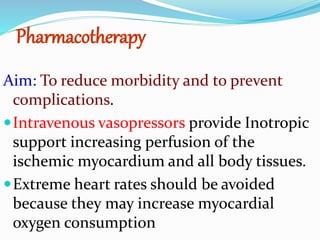
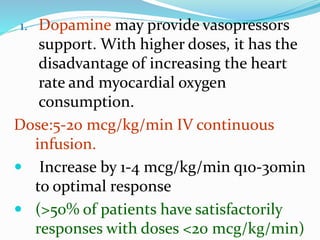
This document discusses various cardiac emergencies including myocardial infarction, angina pectoris, congestive cardiac failure, sudden cardiac arrest, cardiac tamponade, and cardiogenic shock. It provides details on the causes, symptoms, diagnostic measures, and management of these conditions. Specifically, it describes angina pectoris as chest pain caused by partial blockage of the coronary arteries, acute myocardial infarction as damage to the heart muscle caused by a blockage of blood supply, and cardiac tamponade as a life-threatening condition where fluid builds up in the space between the heart muscle and the sac surrounding the heart. The document emphasizes the importance of early recognition, CPR, defibrillation and medications in managing cardiac arrest and