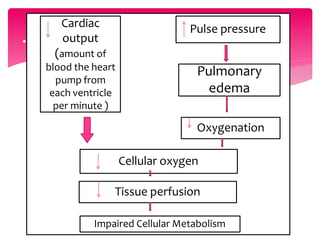
1. Cardiogenic shock occurs when the heart is damaged and unable to pump enough blood to vital organs, which can lead to organ failure.
2. It is caused by conditions like heart attack that damage the heart muscle and impair its ability to contract and pump effectively.
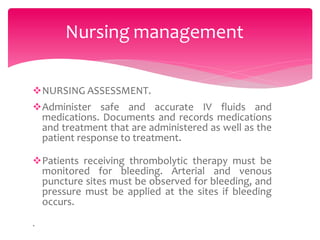
3. Symptoms include low blood pressure, confusion, and reduced urine output as the kidneys are not adequately perfused. Treatment focuses on supporting blood pressure and cardiac function through medications, and procedures like coronary interventions can also be used.