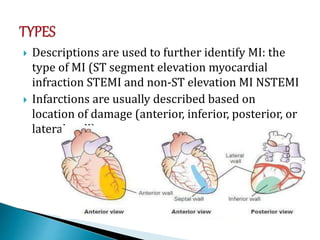
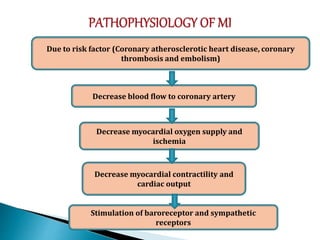
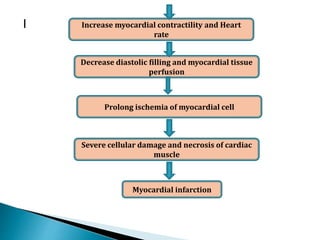
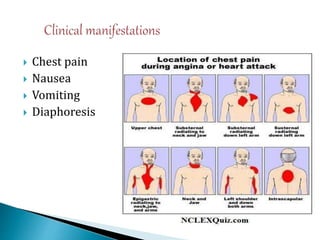
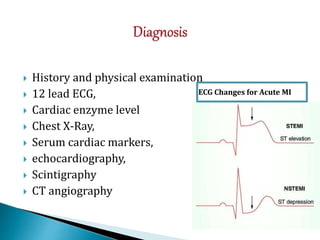
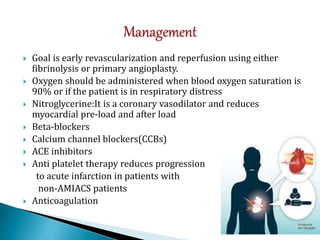
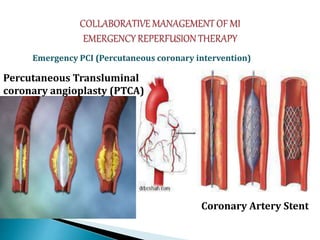
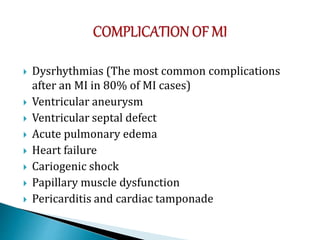
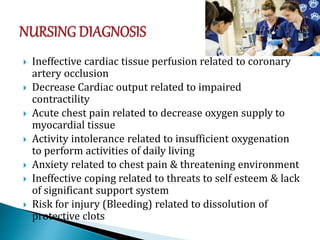
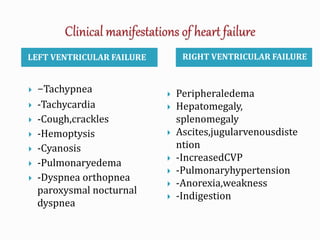
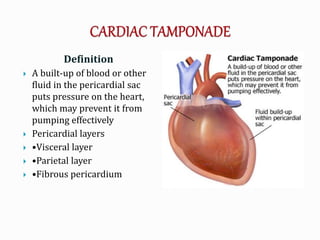
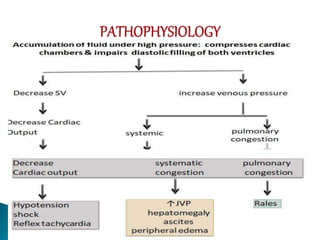
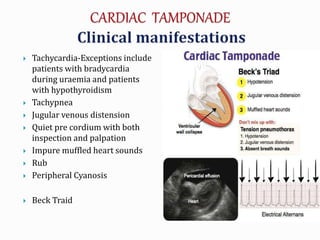
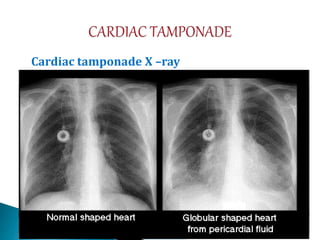
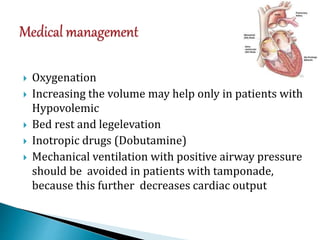
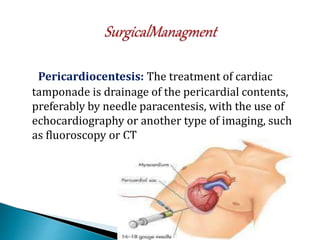
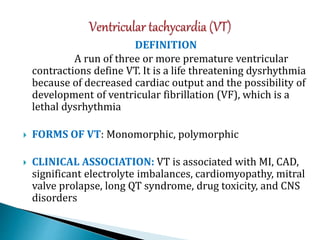
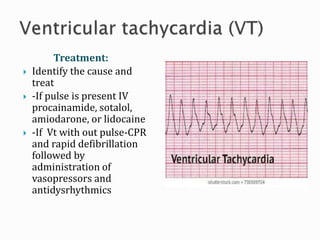
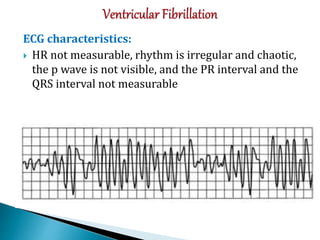
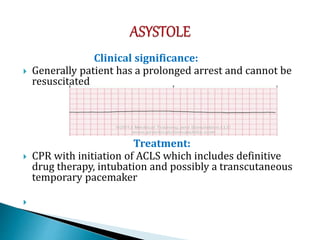
This document provides information about cardiac emergencies presented by Mrs. Shalini, an Assistant Professor of Nursing. It defines cardiac emergencies and lists the learning objectives. The major cardiac emergencies discussed include acute myocardial infarction, heart failure, sudden cardiac death, cardiac tamponade, hypertensive emergencies, and dysrhythmias. For each emergency, the document provides definitions, causes, signs and symptoms, diagnostic tests, management, and nursing care considerations.