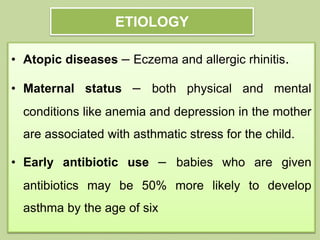
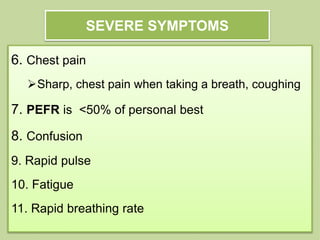
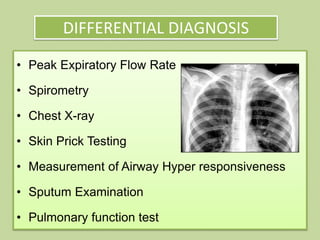
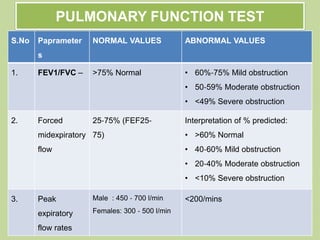
Bronchial asthma is a chronic inflammatory disease of the airways characterized by airflow obstruction, bronchial hyperactivity, and mucus production. It affects 334 million people worldwide and causes 250,000 deaths per year. The disease has genetic and environmental causes and can be triggered by factors like dust, pollen, smoke, and exercise. It is diagnosed based on symptoms, medical history, and pulmonary function tests. Treatment involves bronchodilators, corticosteroids, and other drugs to relieve symptoms and reduce inflammation. Lifestyle changes and avoidance of triggers can also help manage the condition.