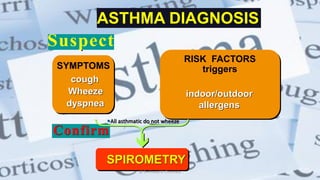
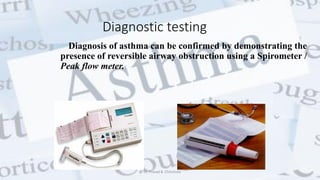
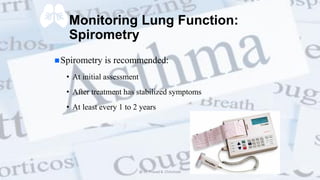
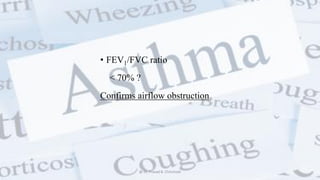
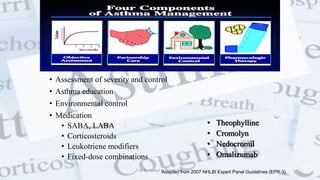
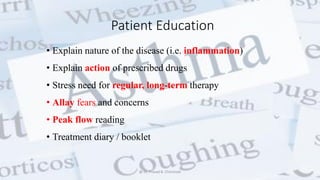
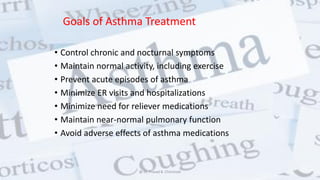
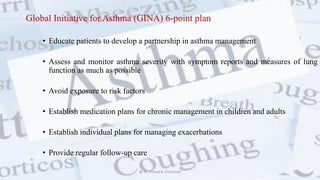
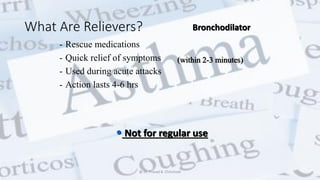
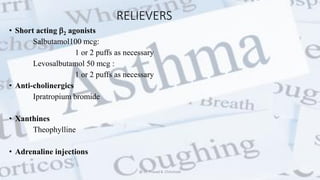
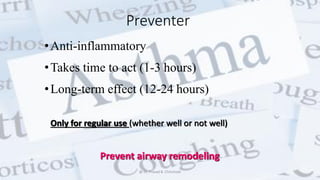
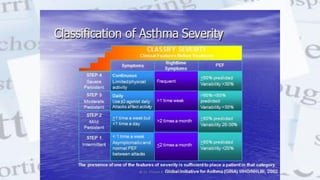
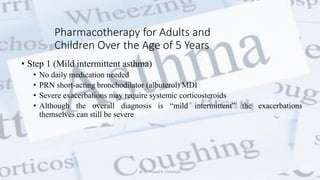
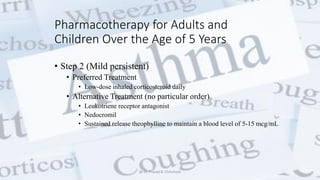
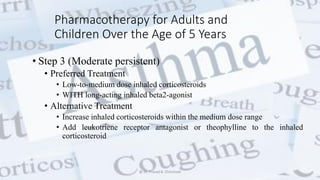
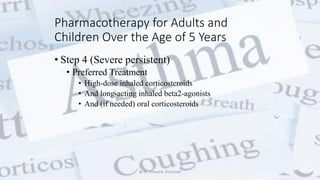
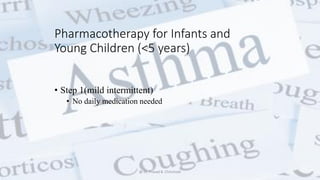
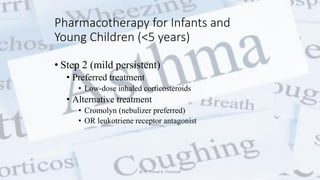
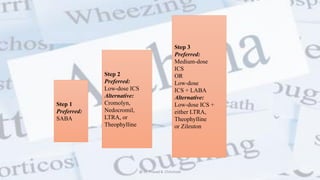
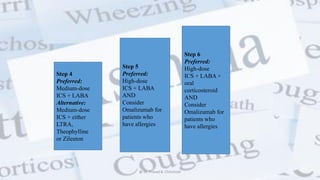
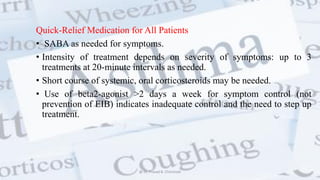
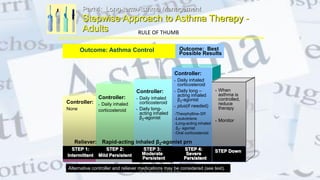
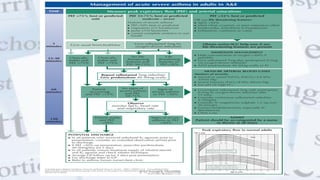
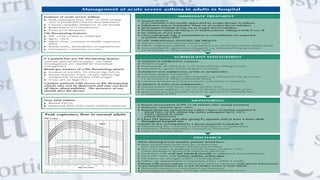
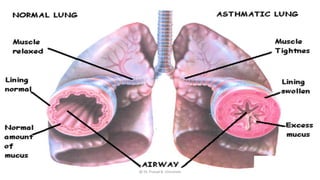
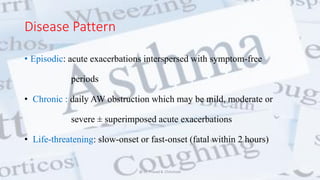
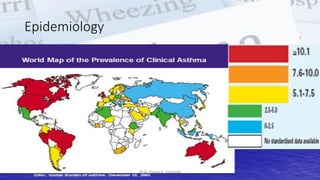
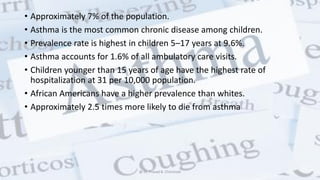
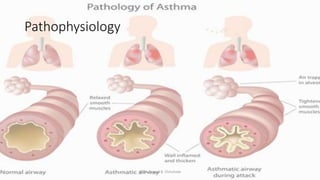
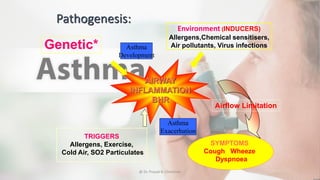
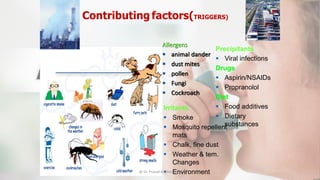
This document provides an overview of asthma, including its definition, pathophysiology, clinical presentation, diagnosis, and management. It defines asthma as a chronic inflammatory disorder of the airways involving various cells. The pathophysiology involves acute and chronic inflammation from triggers like allergens. Diagnosis is based on symptoms, exam, and lung function tests showing reversible airflow obstruction. Management focuses on education, environmental control, and a stepped pharmacologic approach including bronchodilators and inhaled corticosteroids.



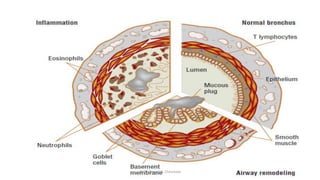
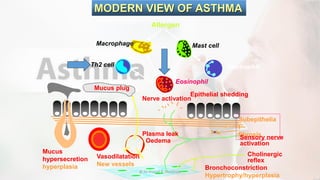
![• Eosinophils migrate to the airways and release inflammatory
mediators (leukotrienes and granule proteins), cytotoxic mediators,
and cytokines.
• T-lymphocyte activation leads to release of cytokines from type 2 T-
helper (TH2) cells that mediate allergic inflammation (interleukin
[IL]-4, IL-5, and IL-13).
• Conversely, type 1 T-helper (TH1) cells produce IL-2 and
interferon- γ that are essential for cellular defense mechanisms.
• Allergic asthmatic inflammation may result from an imbalance
between TH1 and TH2 cells.
@ Dr. Prasad B. Chinchole](https://image.slidesharecdn.com/asthma-180209052441/85/Asthma-20-320.jpg)