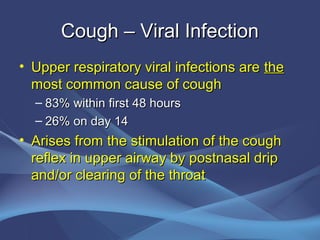
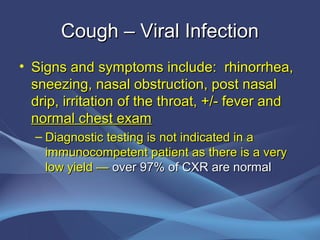
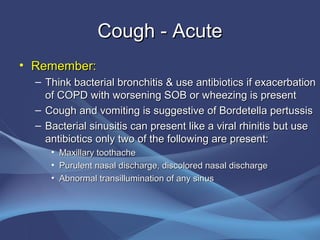
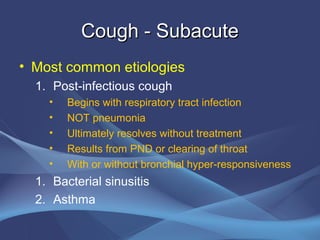
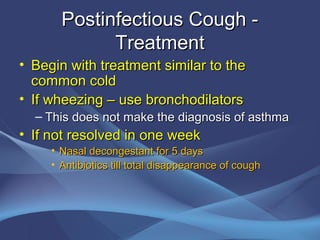
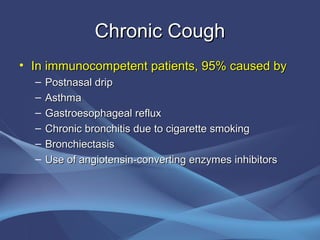
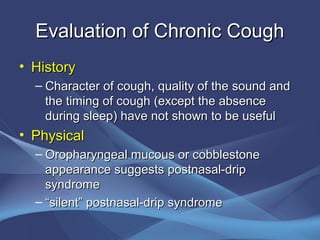
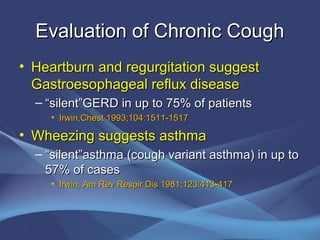
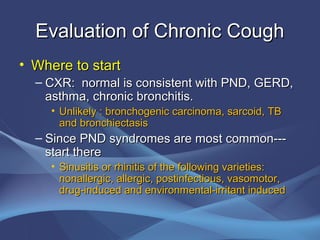
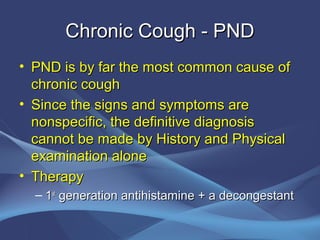
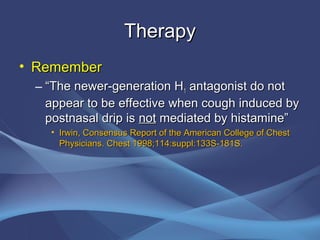
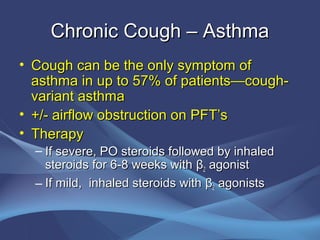
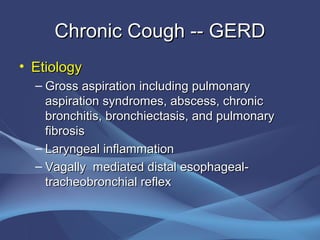
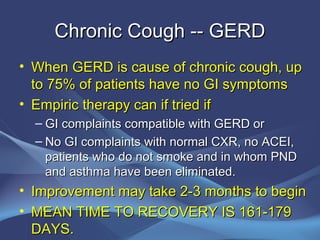
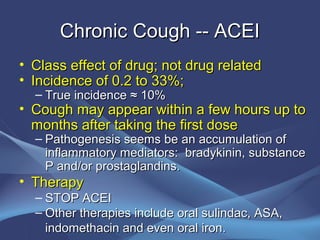
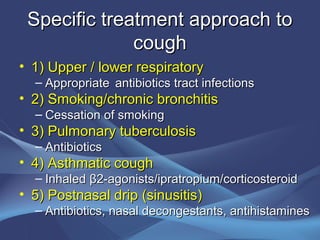
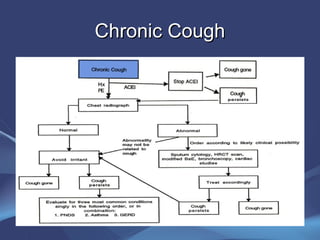
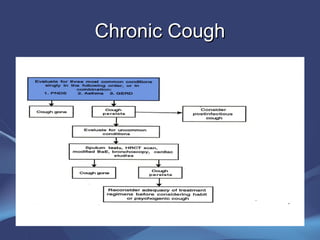
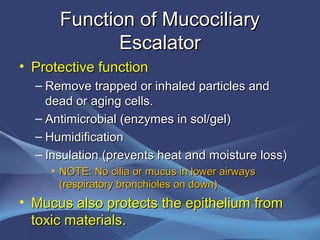
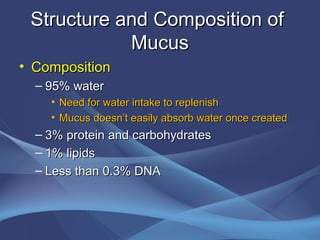
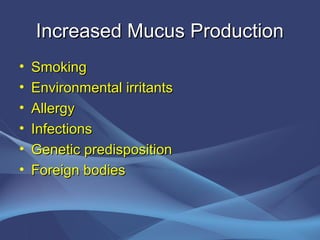
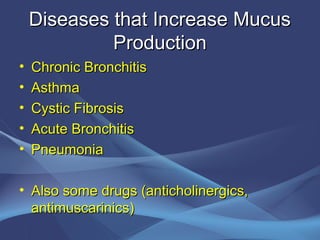
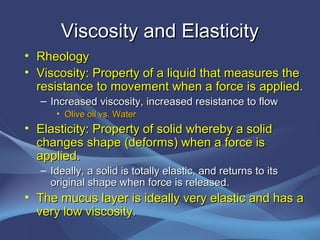
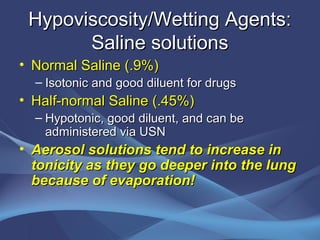
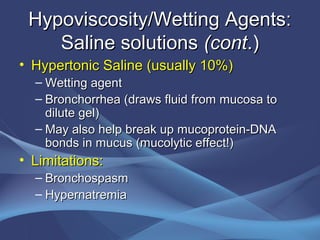
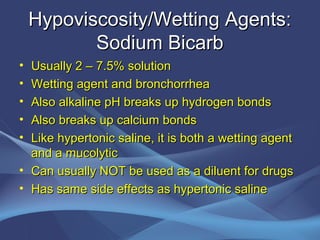
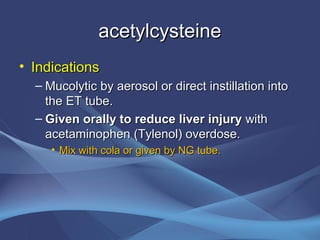
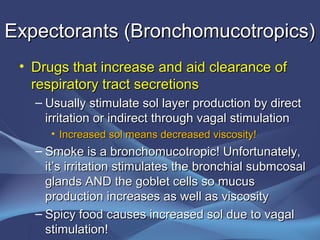
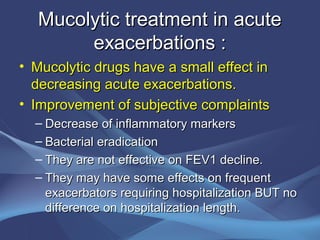
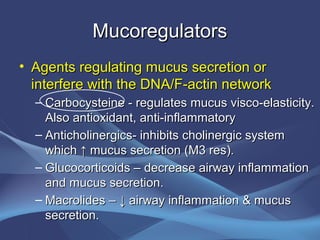
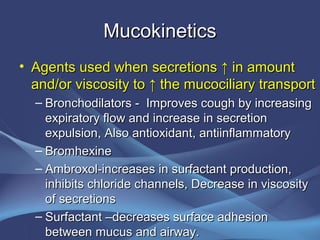
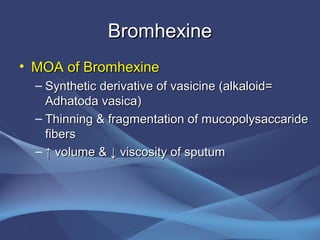
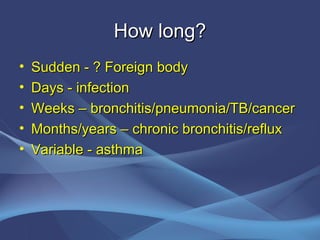
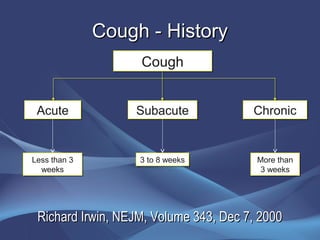
This document discusses the treatment of cough. It begins by classifying cough based on duration as acute (less than 3 weeks), subacute (3-8 weeks), or chronic (more than 3 weeks). For acute cough, the most common causes are viral infections, sinusitis, pertussis, COPD exacerbations, and allergies. Post-infectious cough can last 1-2 weeks. Chronic cough is often caused by postnasal drip, asthma, gastroesophageal reflux, or smoking-related chronic bronchitis. The document provides guidance on evaluating and treating cough based on duration and suspected etiology. Emphasis is placed on treating the underlying cause rather than just suppressing cough symptoms.

![Cough - Acute
• Most common causes
– Common cold [viral]
– Acute bacterial sinusitis
– Pertussis
– Exacerbation of COPD
– Allergic rhinitis
– Rhinitis secondary to environmental irritants](https://image.slidesharecdn.com/cough-130202224209-phpapp01/85/Cough-5-320.jpg)