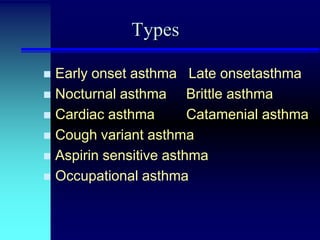
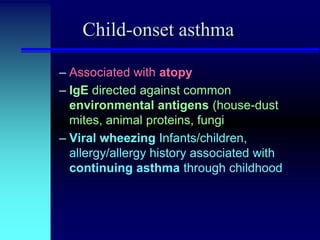
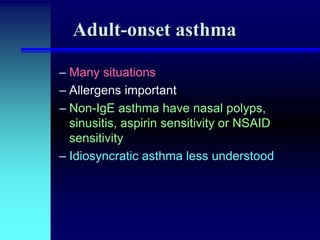
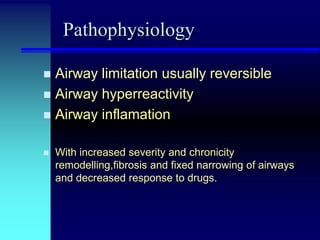
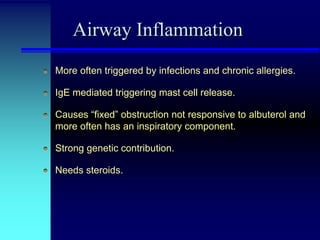
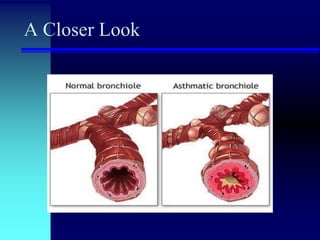
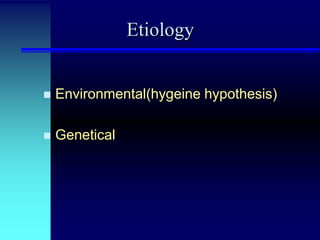
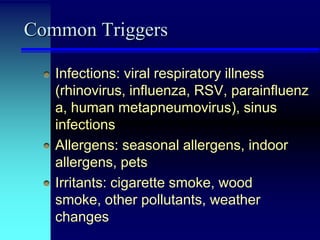
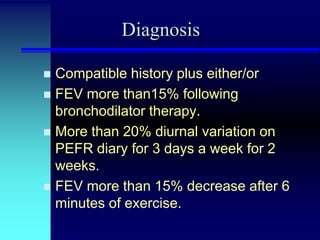
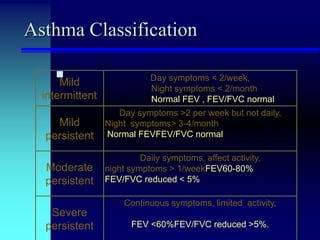
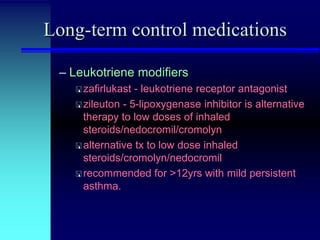
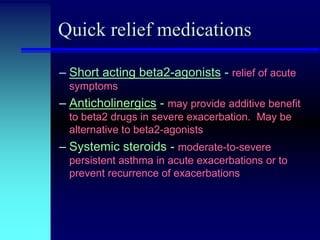
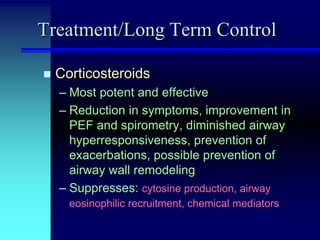
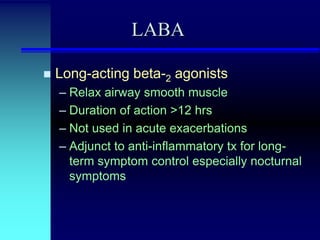
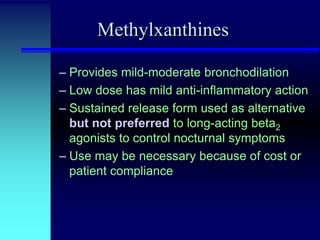
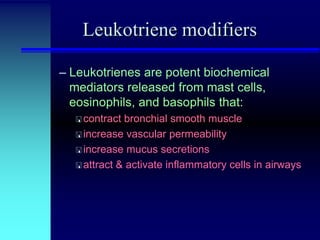
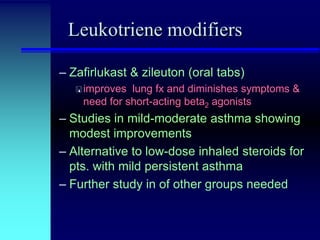
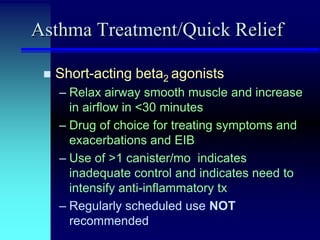
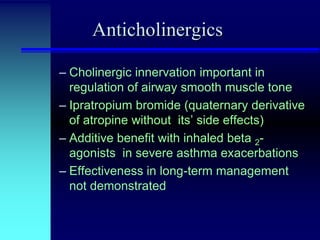
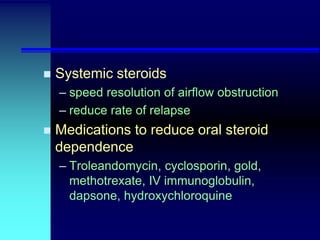
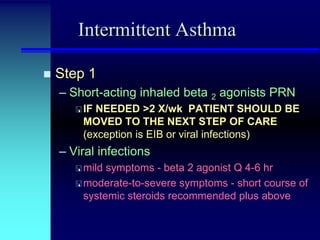
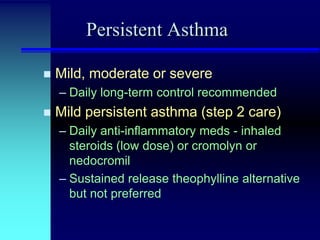
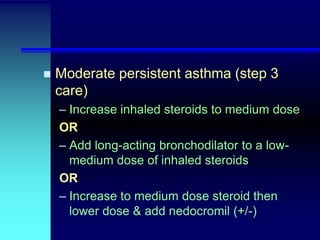
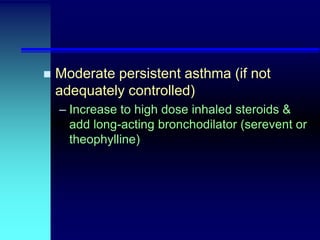
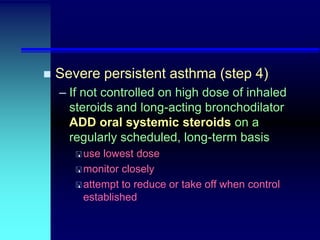
Asthma is a chronic inflammatory disorder of the airways characterized by variable airflow obstruction and airway hyperresponsiveness. It has different classifications based on severity and is treated through long-term control medications like inhaled corticosteroids and bronchodilators as well as quick-relief medications for acute symptoms. The pathophysiology involves airway inflammation, remodeling, and hyperresponsiveness triggered by allergens, infections, and other environmental factors.