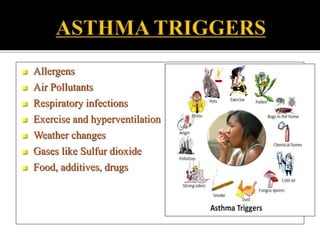
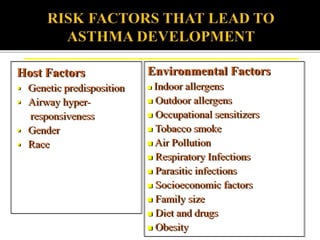
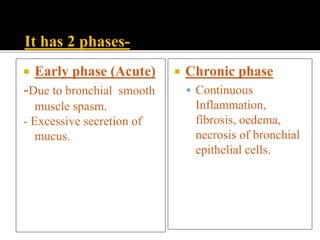
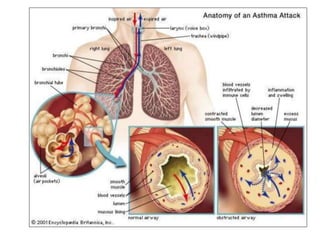
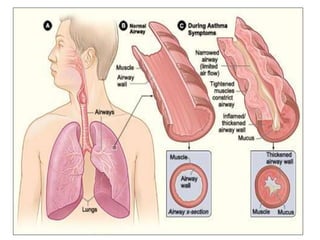
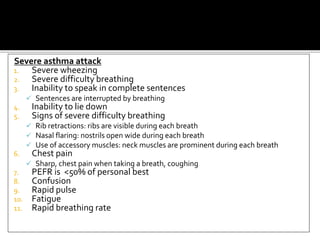
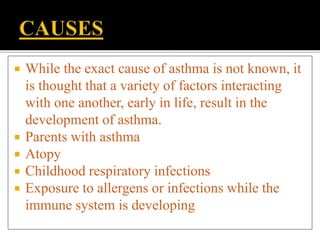
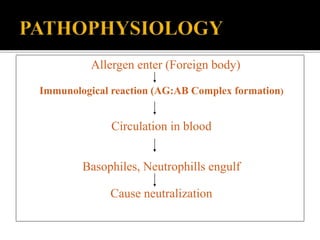
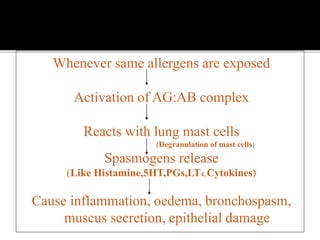
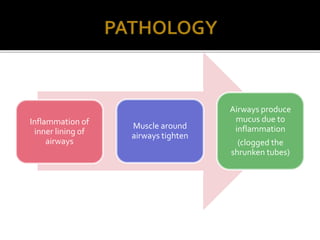
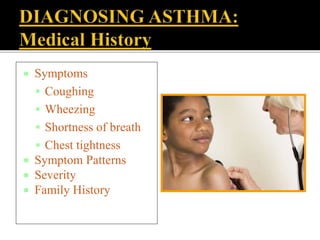
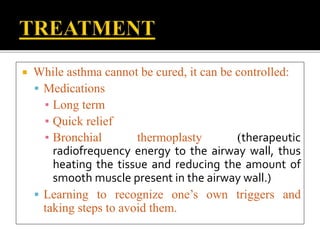
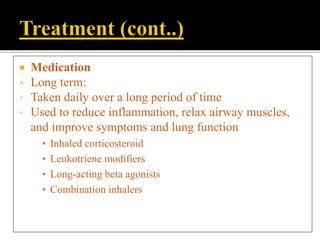
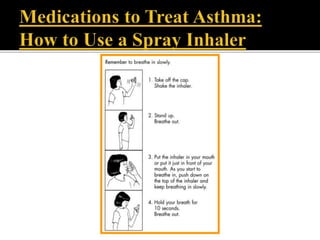
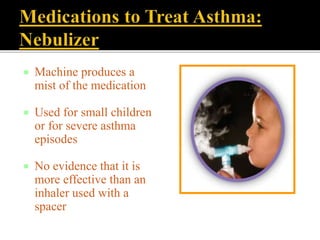
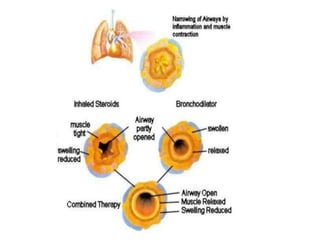
Bronchial asthma is a chronic inflammatory disease of the airways characterized by recurrent episodes of wheezing, breathlessness, chest tightness, and coughing. Key symptoms include coughing, especially at night, wheezing, and shortness of breath. Asthma affects over 300 million people worldwide and is caused by a combination of genetic and environmental factors. While there is no cure, asthma can be effectively controlled through medication like inhaled corticosteroids and bronchodilators, and by avoiding triggers.