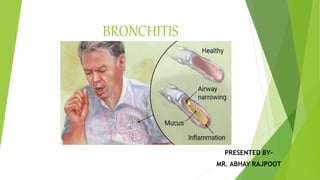
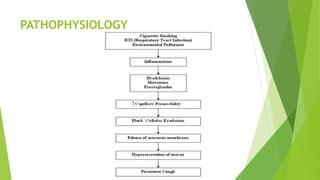
Bronchitis is an inflammation of the bronchial tubes causing cough, mucus production, and symptoms like shortness of breath and chest tightness. It can be classified as acute, often caused by viruses, or chronic, typically resulting from smoking and environmental irritants. Diagnosis may involve chest x-rays and sputum tests, with management including bronchodilators, corticosteroids, and lifestyle changes for prevention.