This document provides an overview of asthma including its incidence, etiology, pathophysiology, clinical manifestations, diagnosis, and management. Some key points:
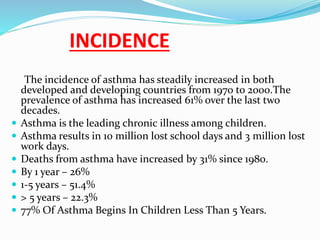
- Asthma prevalence has increased 61% over the last two decades and it is the leading chronic illness among children.
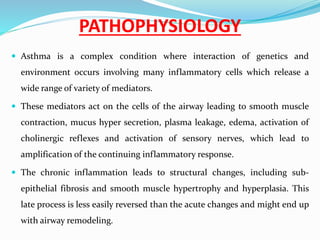
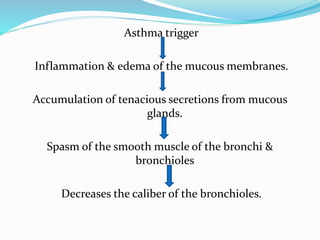
- It is caused by airway inflammation and obstruction from factors such as allergens, infections, pollutants, and psychosocial stress.
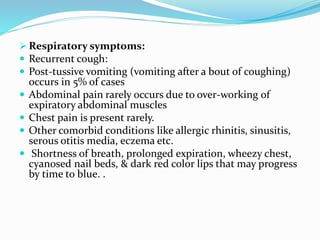
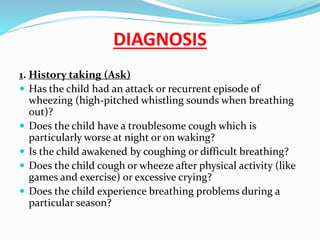
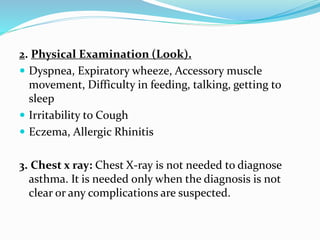
- Symptoms include dyspnea, wheezing, and cough. Diagnosis involves patient history, physical exam, and sometimes chest X-rays.
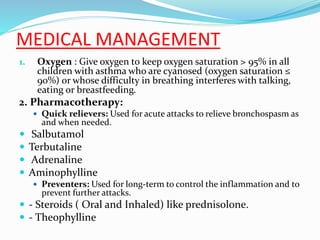
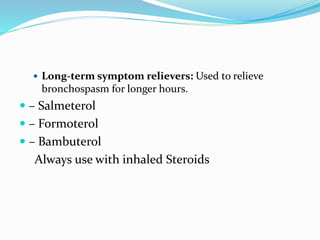
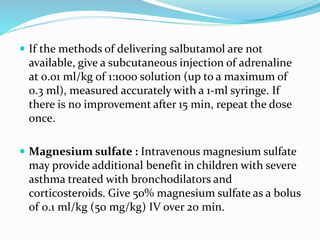
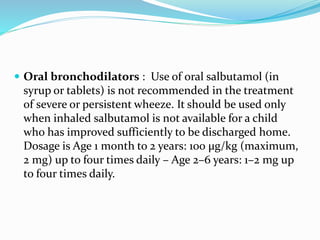
- Treatment involves quick relievers for acute attacks, preventers to control inflammation, and environmental control/patient education. Nursing care focuses on education