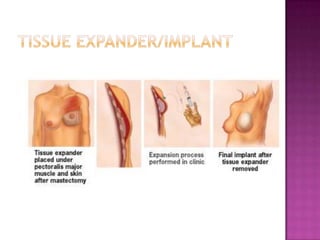
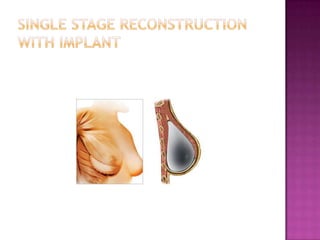
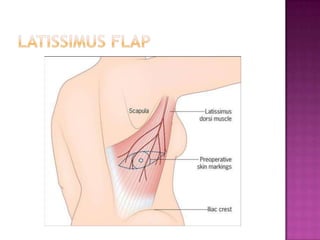
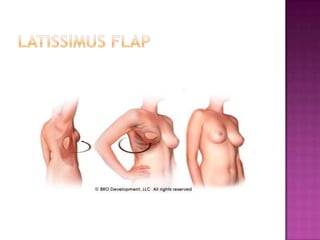
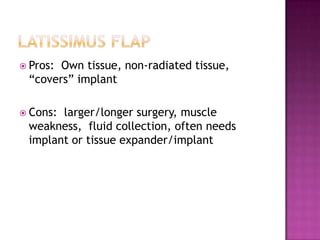
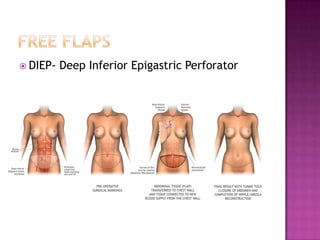
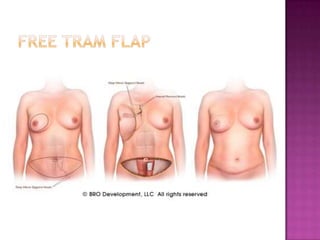
Dr. Vanessa Voge discusses various breast reconstruction options available to women after mastectomy due to breast cancer, highlighting advancements that have improved patient choices. The document details different types of reconstructive surgeries, timing considerations, and challenges associated with each option, emphasizing the importance of individualized treatment plans. Additionally, it addresses the impact of cancer treatments on reconstruction and the psychological and emotional dimensions of undergoing these procedures.