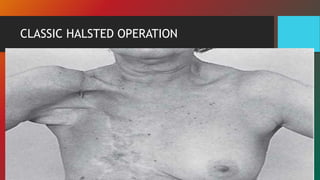
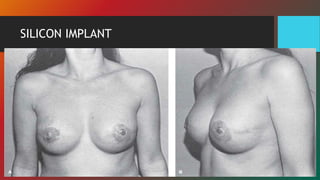
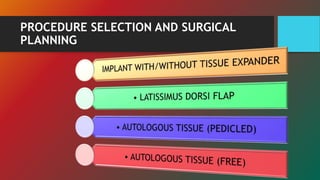
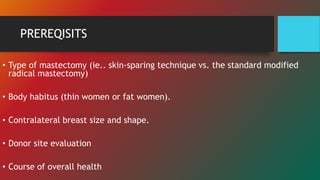
The document discusses the evolution and techniques of breast reconstruction, detailing approaches using implants and autologous tissue, notably the latissimus dorsi and TRAM flaps. It emphasizes the role of general surgeons in planning and executing these procedures while highlighting patient considerations and post-operative results. Historical references illustrate the advancements in surgical methods and their impacts on reconstruction outcomes.