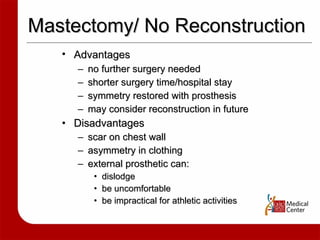
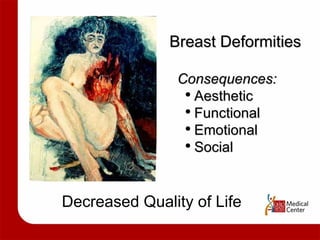
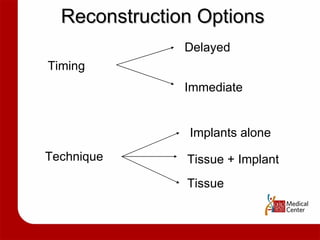
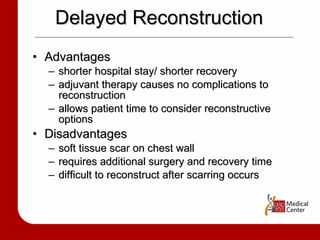
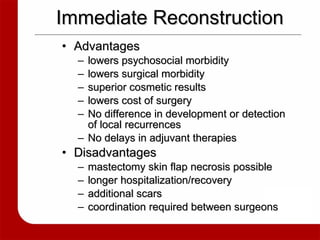
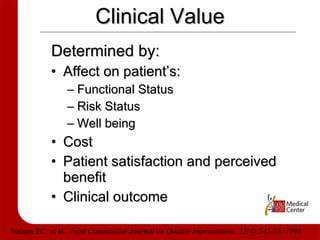
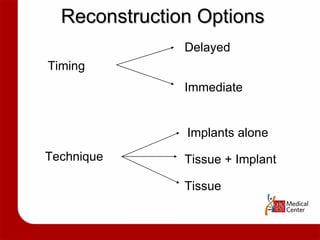
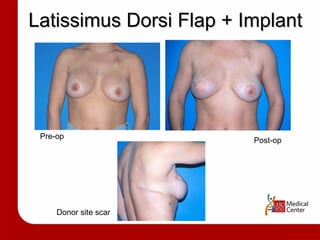
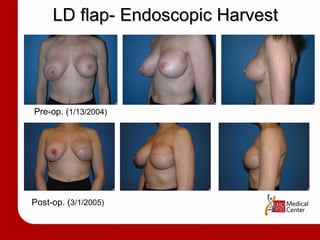
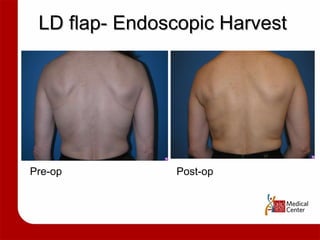
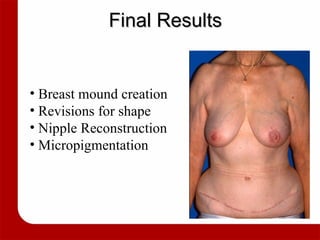
1. The document discusses various options for breast reconstruction after mastectomy, including immediate versus delayed reconstruction and the use of tissue flaps, implants, or a combination.
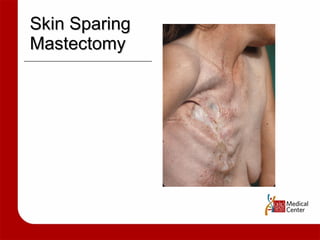
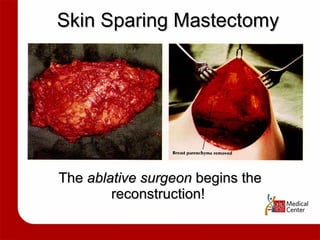
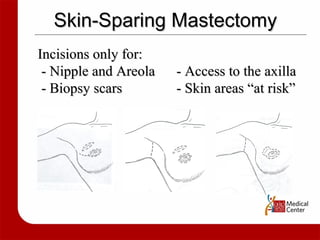
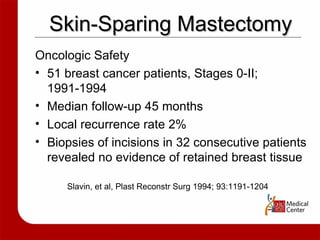
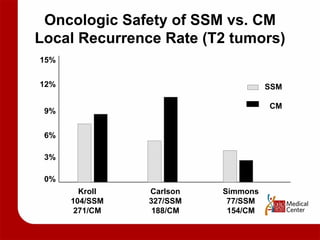
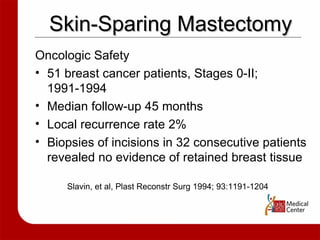
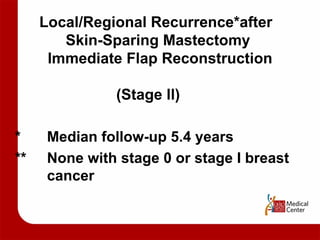
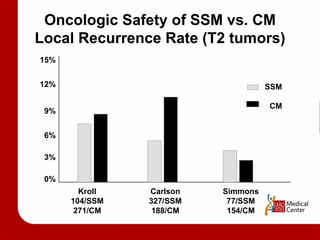
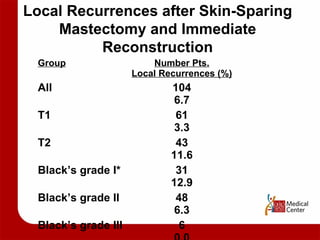
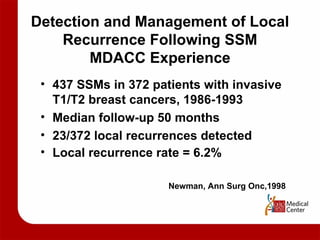
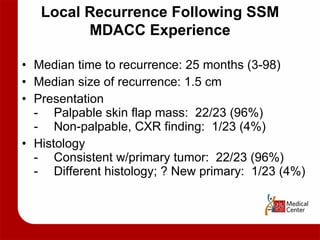
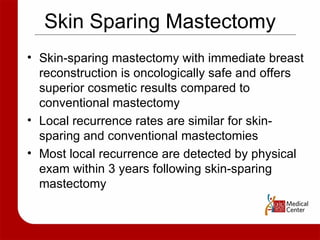
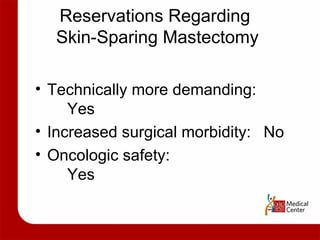
2. Skin-sparing mastectomy is described as oncologically safe based on studies finding local recurrence rates similar to conventional mastectomy and most recurrences detected within 3 years.
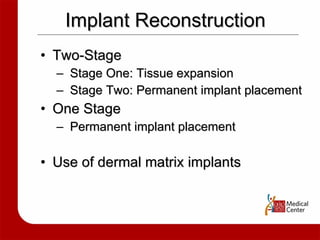
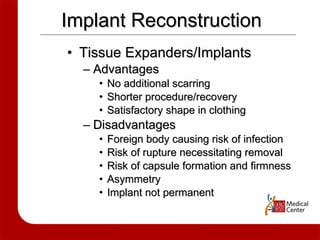
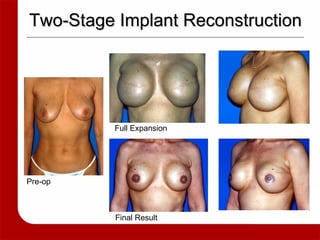
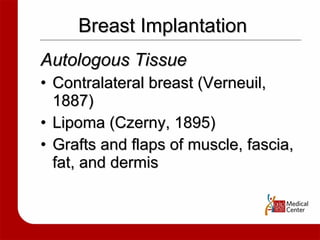
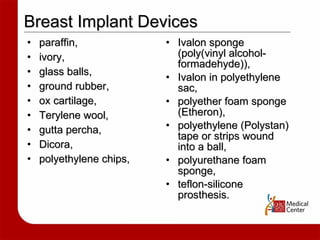
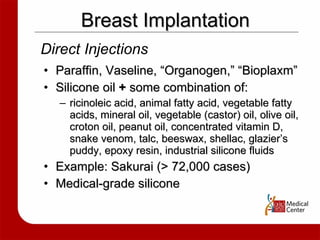
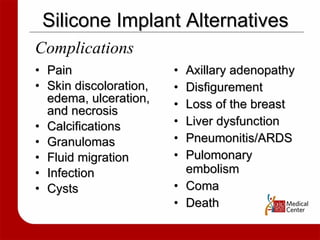
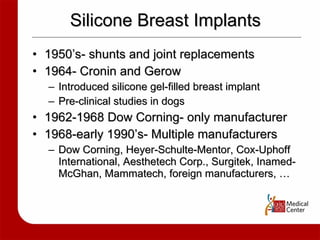
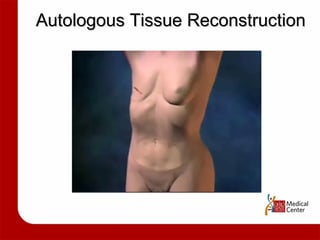
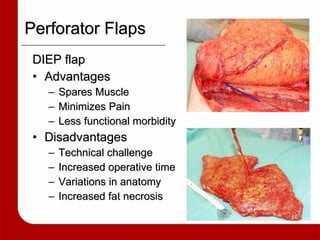
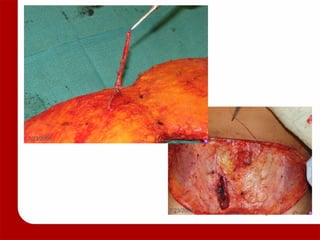
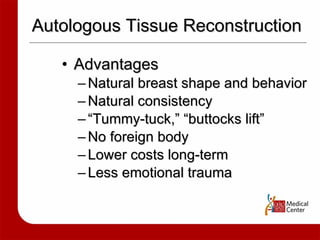
3. Autologous tissue reconstruction is discussed as having advantages like a natural appearance but also longer recovery, while implant reconstruction has shorter procedure time but risks like infection or capsular contracture.