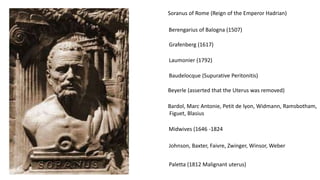
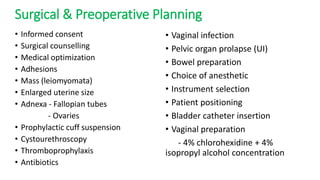
This document discusses the history and techniques of vaginal hysterectomy. It provides details on the procedure including patient positioning, instrumentation, surgical steps like incising the vaginal mucosa and entering the pelvic spaces, clamping and suturing of ligaments, and uterine removal. Post-operative complications are also reviewed. The document serves as a reference for gynecologists performing this common gynecological surgery.