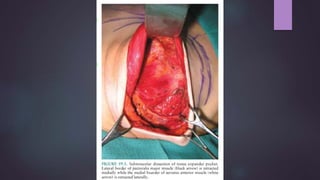
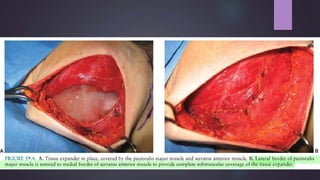
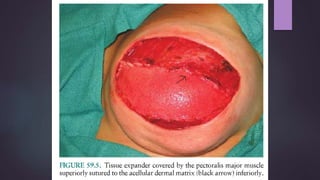
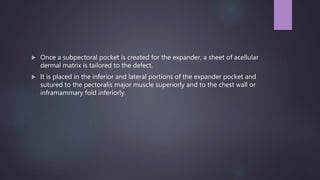
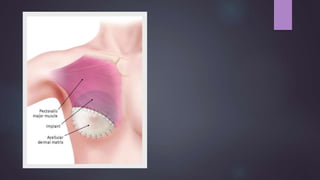
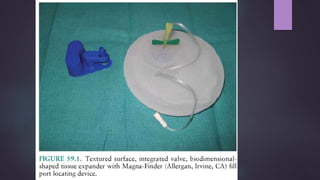
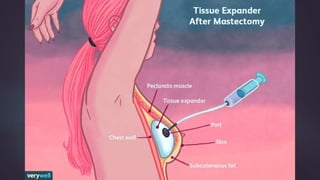
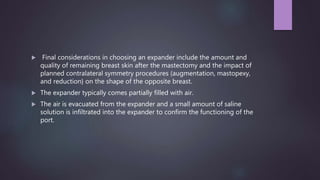
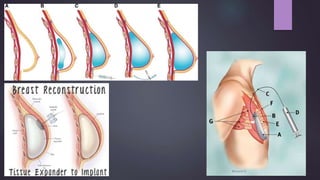
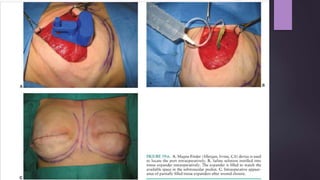
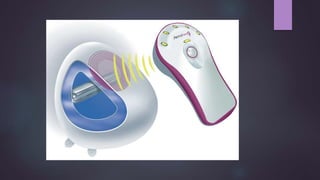
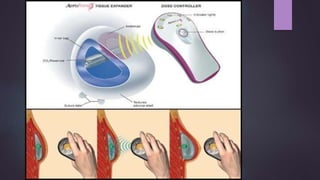
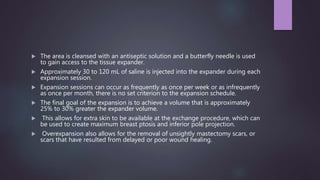
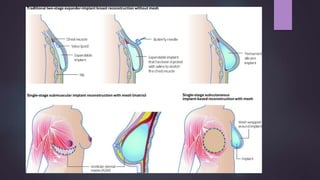
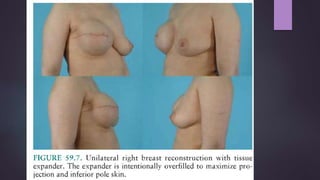
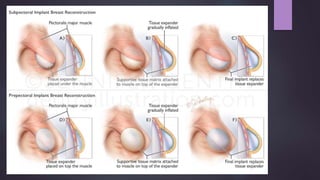
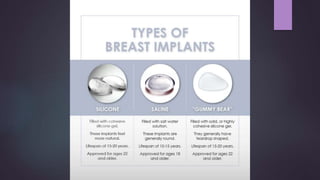
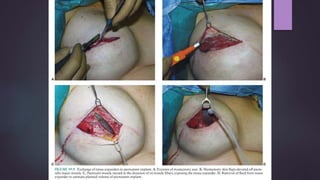
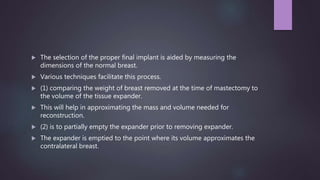
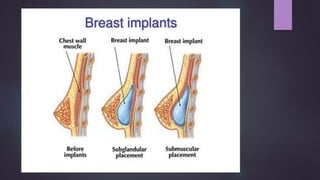
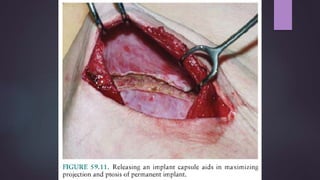
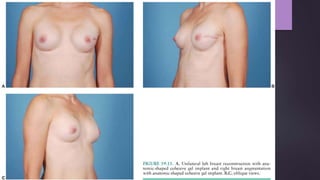
This document discusses techniques for breast reconstruction using prosthetic implants. It describes patient selection criteria, timing considerations for reconstruction, surgical techniques including tissue expansion and implant exchange, and goals for creating symmetry. The key steps are patient education, tissue expansion over multiple sessions to achieve adequate size, and careful implant selection and positioning to match the other breast.