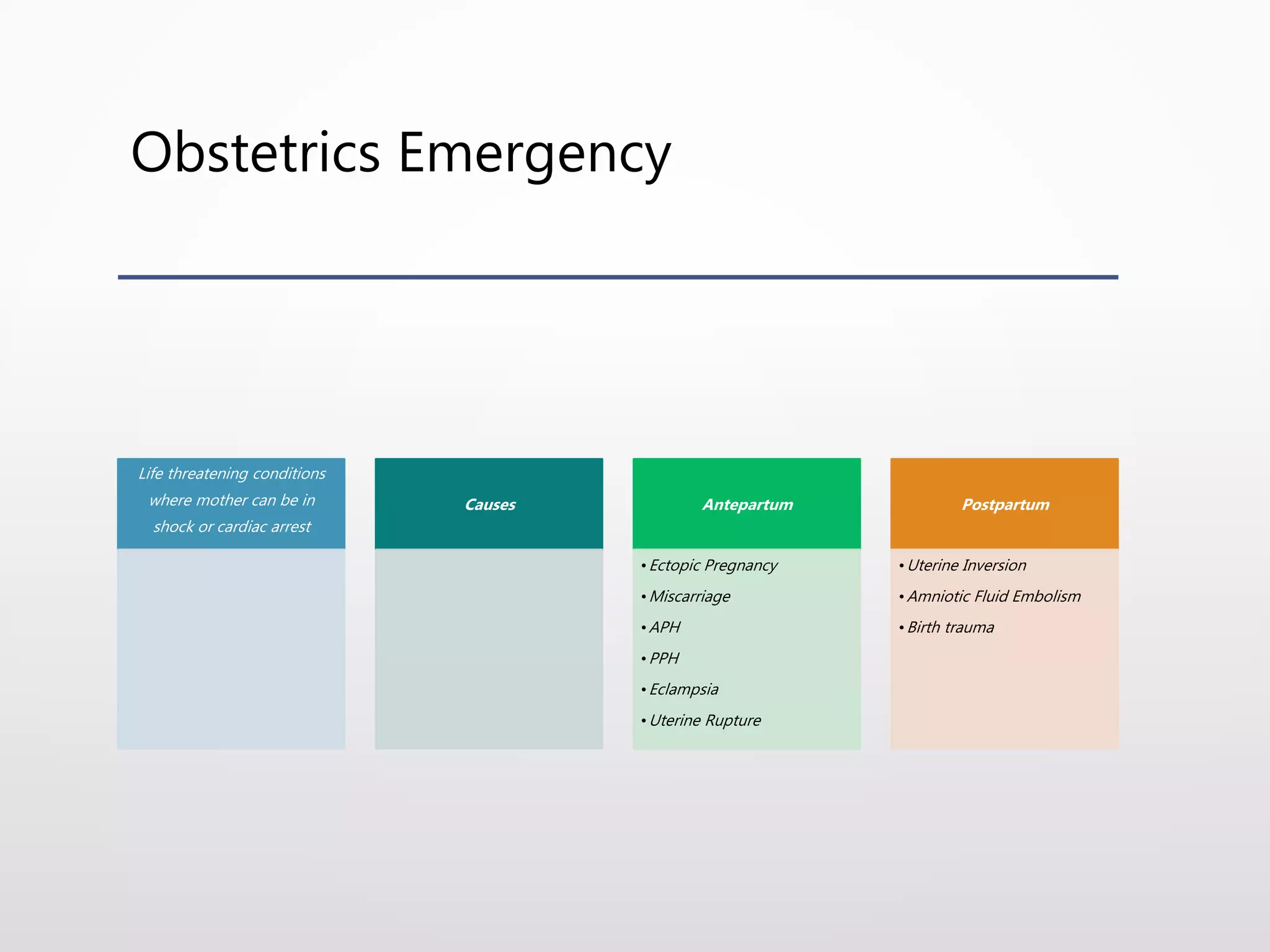
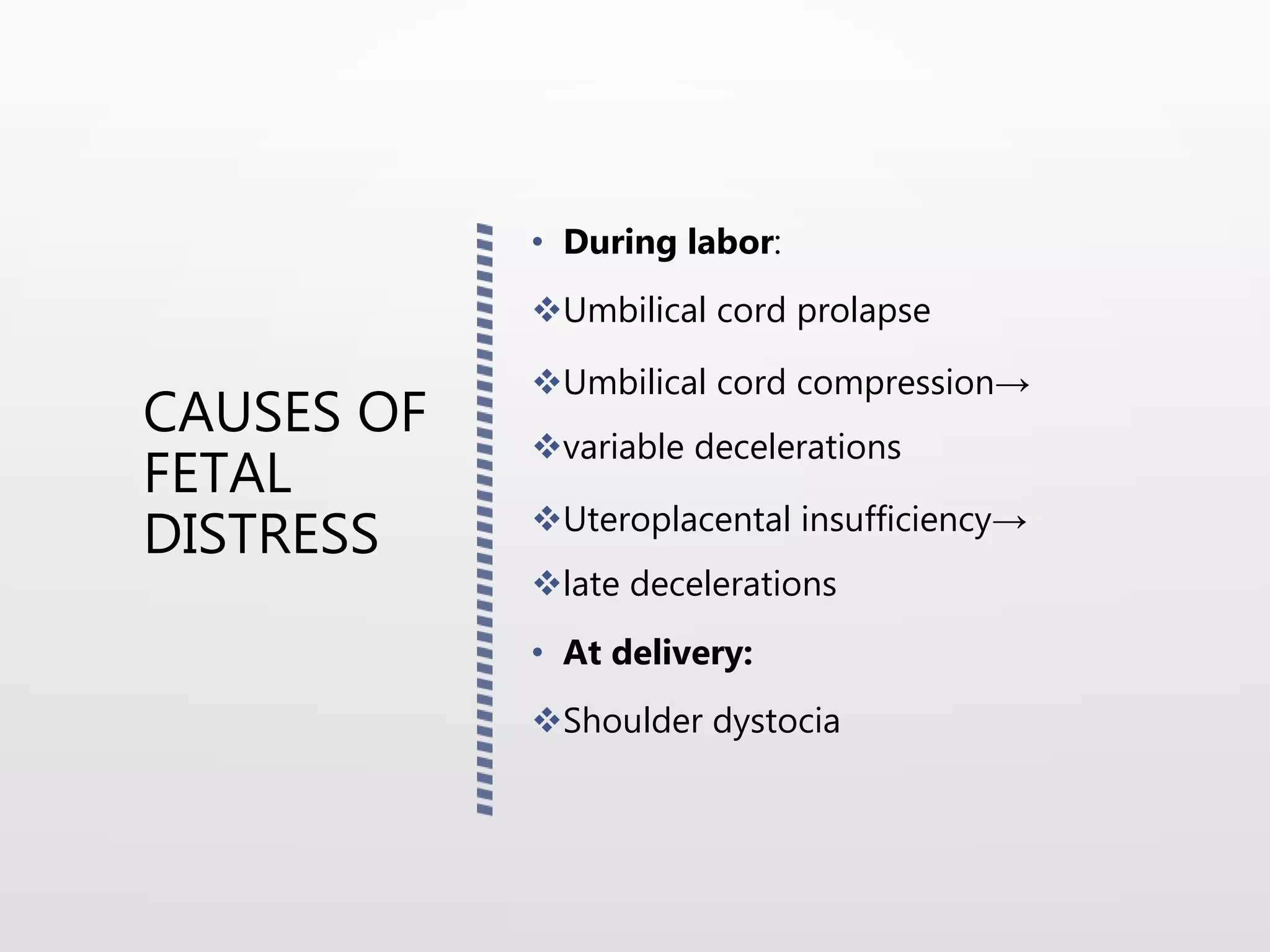
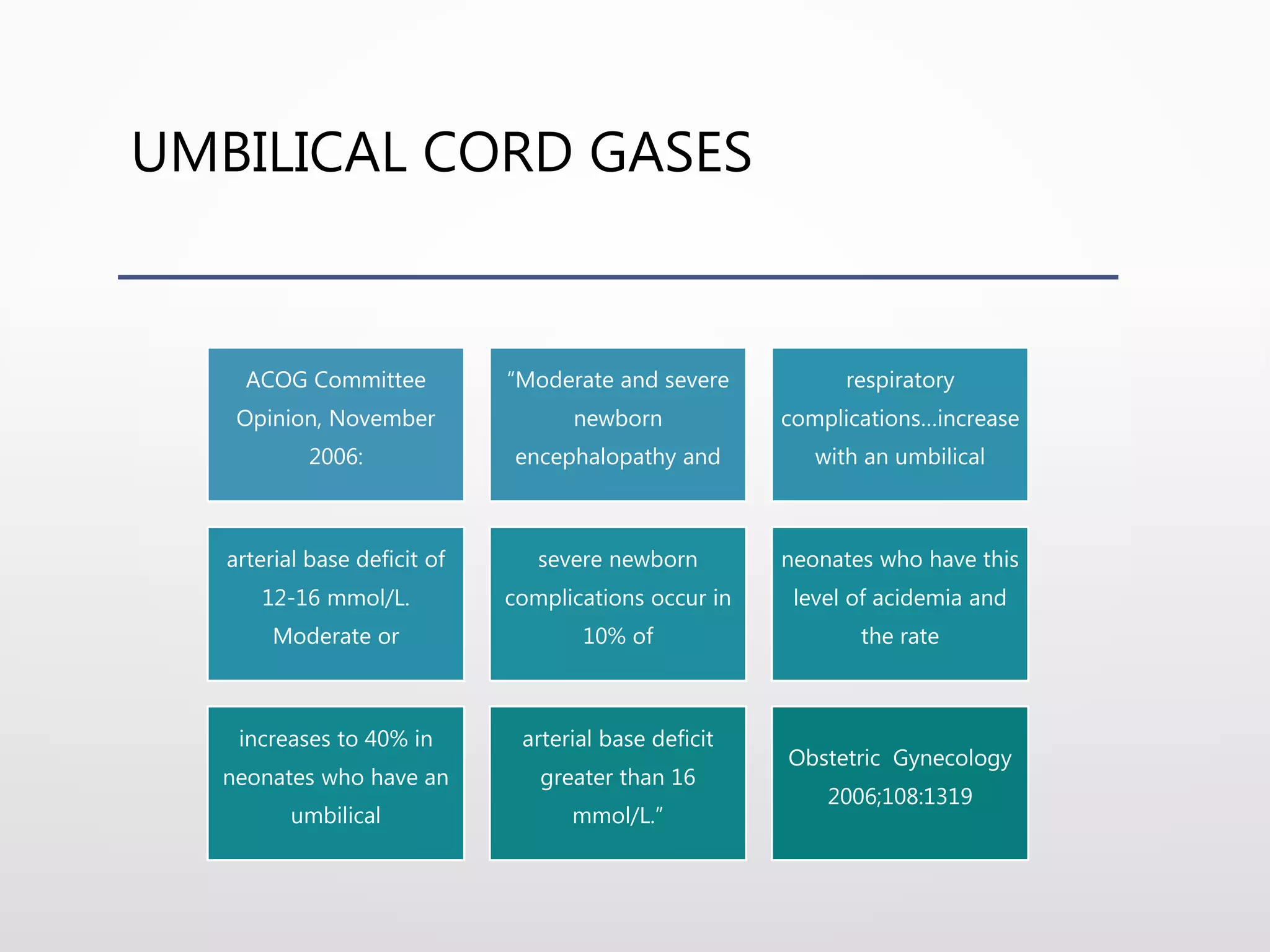
The document discusses various life-threatening obstetric emergencies, including antepartum and postpartum complications such as ectopic pregnancy, uterine rupture, and amniotic fluid embolism. It emphasizes the importance of rapid response, proper management techniques, and the need for a skilled medical team to avoid rapid deterioration of the patient's condition. Additionally, it outlines specific management strategies, diagnosis criteria, and potential interventions related to these emergencies.