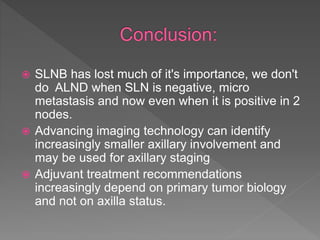
- Sentinel lymph node biopsy (SLNB) is an important prognostic factor in breast cancer as it allows detection of cancer spread to axillary lymph nodes.
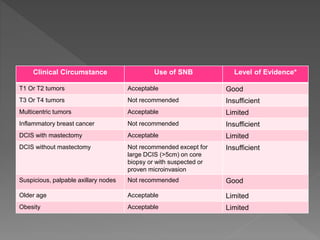
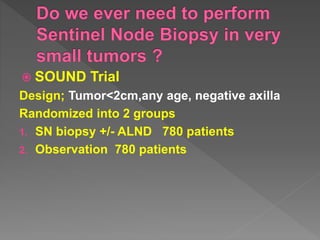
- SLNB is recommended for early-stage T1-T2 tumors without clinically detectable lymph node involvement but is not recommended for larger T3-T4 tumors or inflammatory breast cancer.
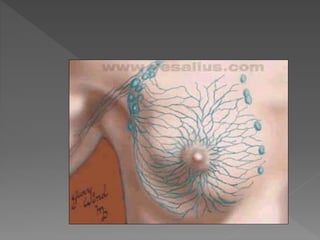
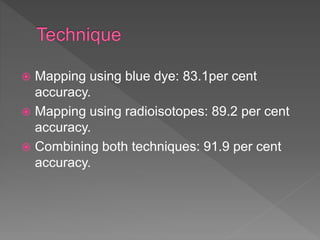
- SLNB accuracy can be improved to over 90% by using blue dye mapping and radioisotope tracing techniques together. A negative SLNB result can spare patients from additional axillary lymph node dissection but a positive result may require further treatment.