1. Oncoplastic breast surgery (OPBS) combines oncological surgery with plastic surgery techniques to allow for wide excision of breast cancer tumors while maintaining the natural shape of the breast.
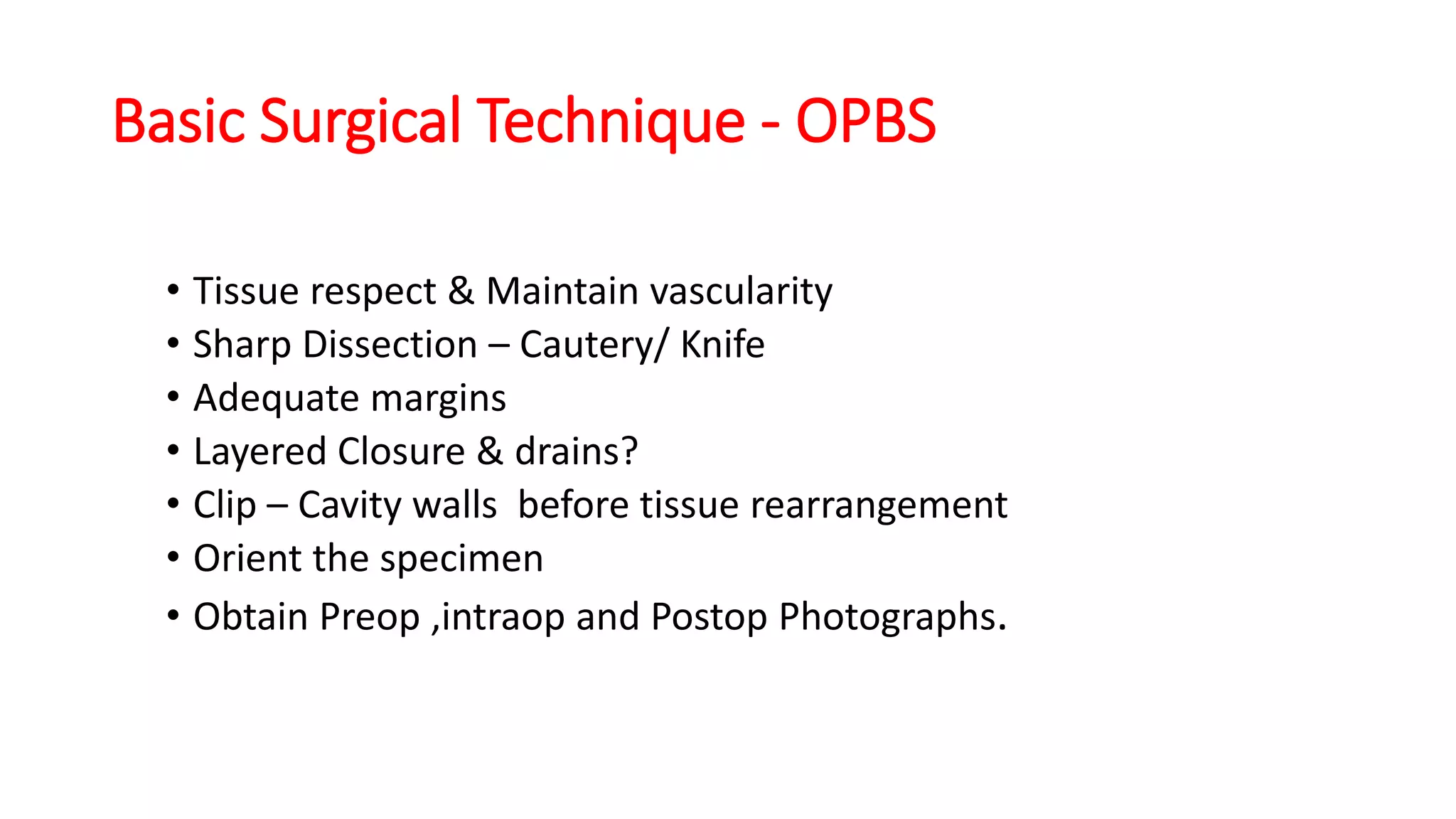
2. OPBS techniques have evolved since the 1980s and can be used for breast-conserving surgery, post-mastectomy reconstruction, or correction of defects after standard breast-conserving surgery.
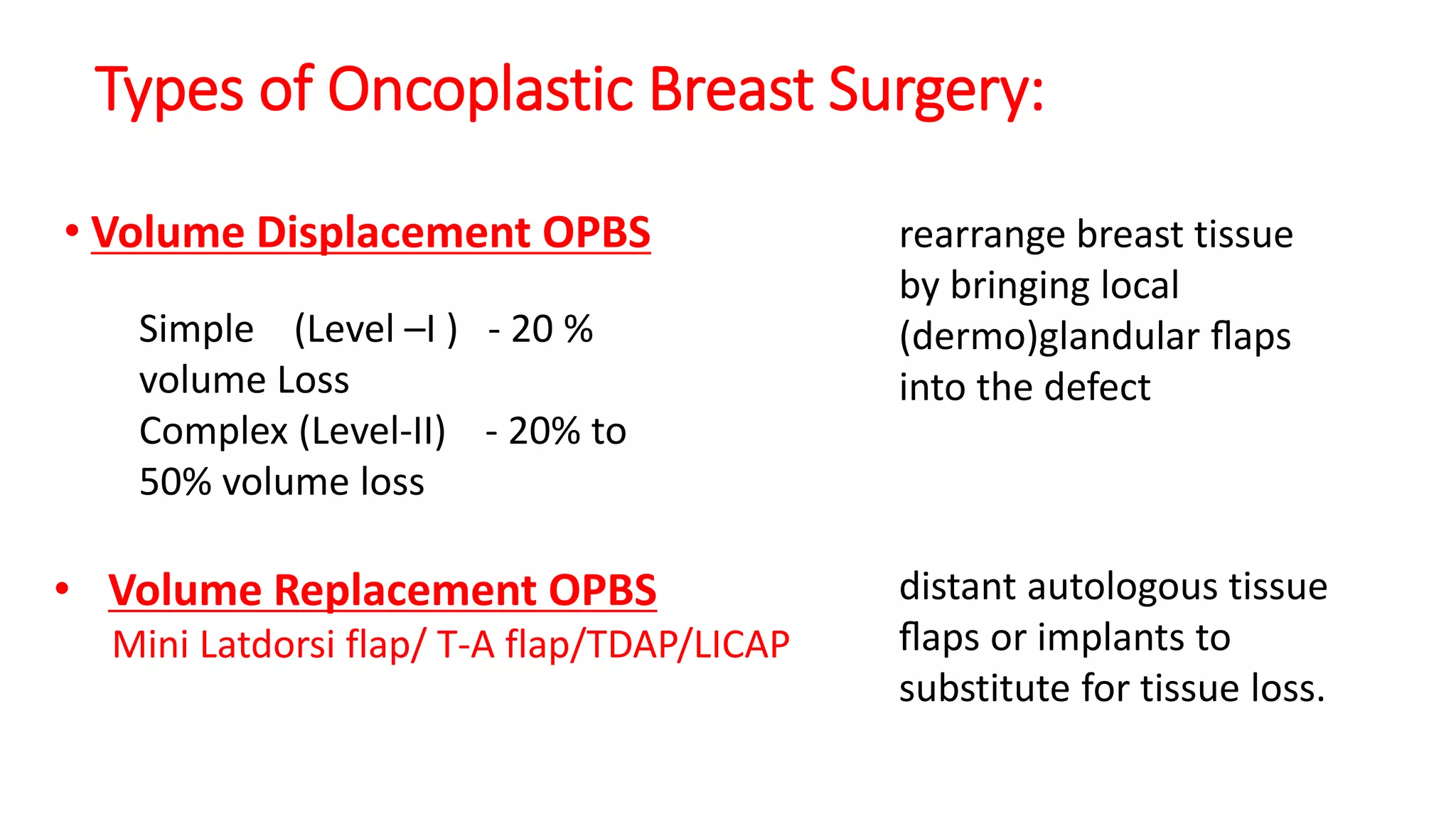
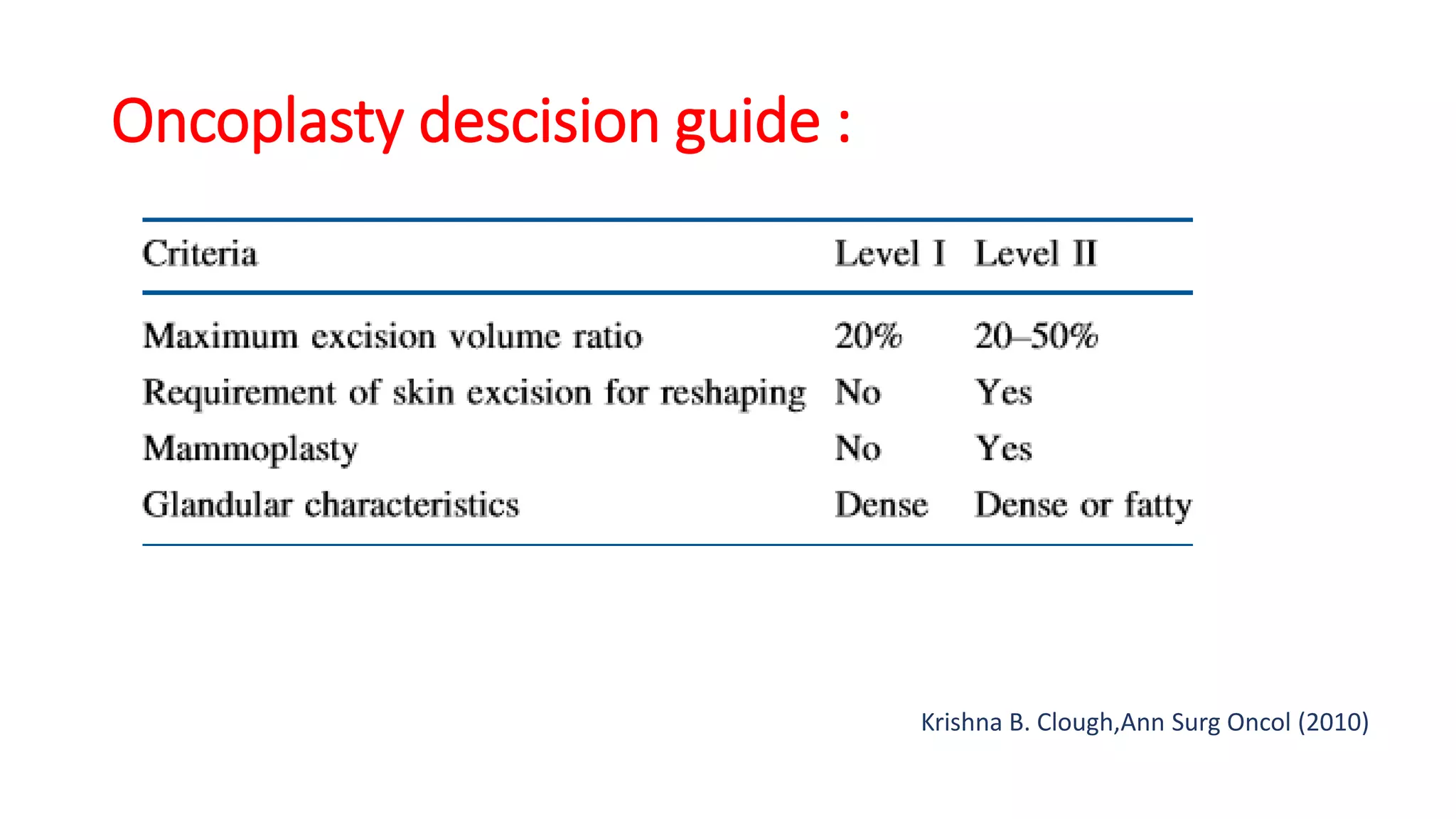
3. OPBS is generally indicated for early-stage breast cancers less than 4cm and can extend the use of breast-conserving surgery to larger tumors. Selection depends on factors like excision volume, tumor location, and breast density.