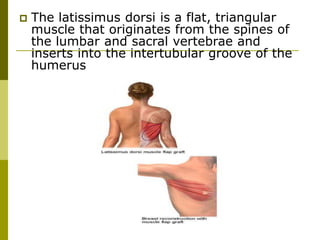
The document discusses breast reconstruction, outlining its objectives, historical advancements, surgical options, and patient selection criteria. It highlights various methods including autogenous and alloplastic reconstructions, the pros and cons of each, as well as considerations for timing and patient factors affecting outcomes. Additionally, it addresses complications and the importance of psychosocial factors in the patient selection process.