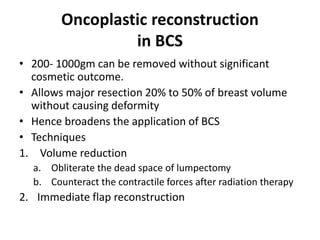
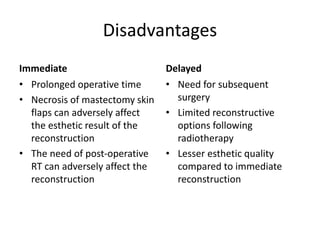
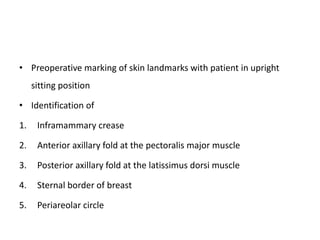
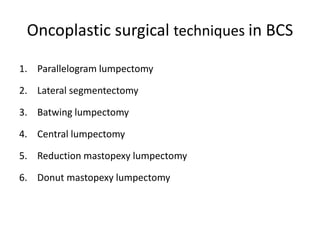
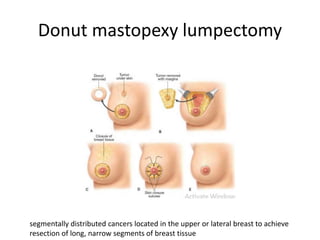
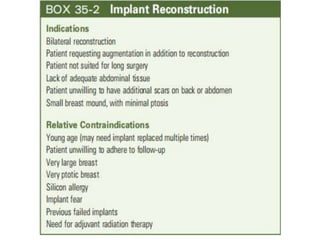
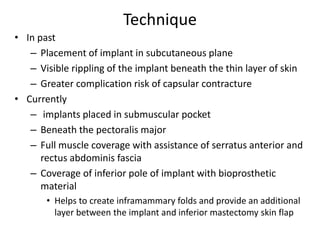
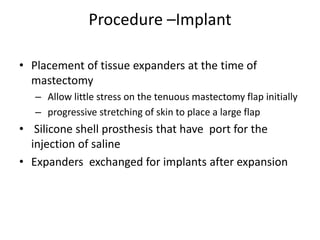
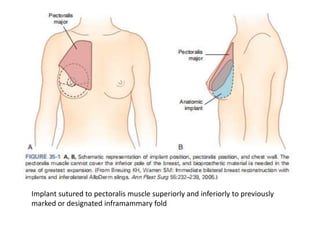
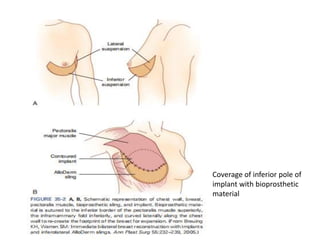
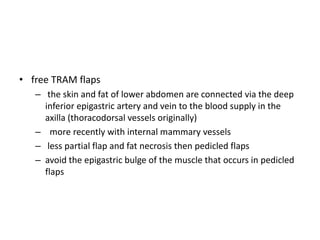
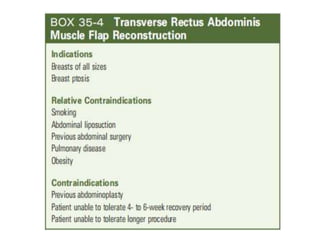
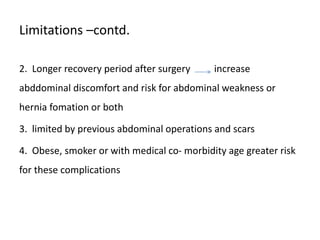
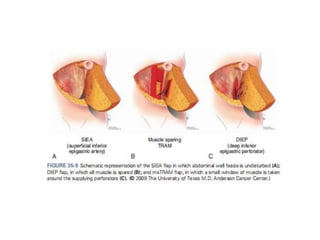
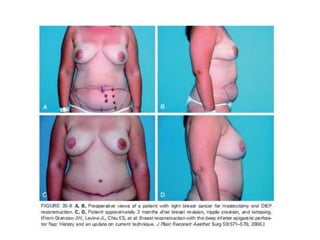
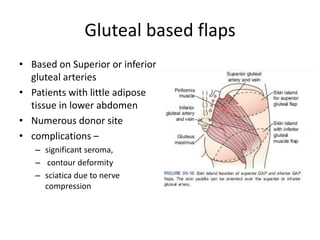
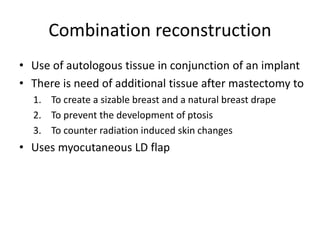
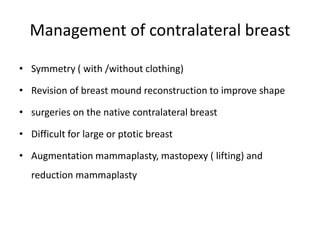
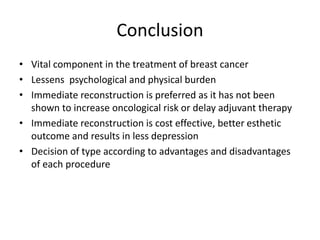
Oncoplastic breast surgery aims to maintain breast appearance and quality of life while achieving oncological effectiveness. It combines breast cancer surgery with plastic surgery techniques to reconstruct partial or whole breasts. A multidisciplinary team is involved in patient selection and planning. Techniques include volume displacement or volume replacement to allow tumor resection while minimizing deformity. Reconstruction can be done immediately or delayed, with each approach having advantages and disadvantages. Autologous flaps from the abdomen, back, or thighs are commonly used though implant reconstruction is also an option. Nipple reconstruction further improves cosmetic outcomes. Oncoplastic surgery provides improved cosmesis over conventional surgery alone.