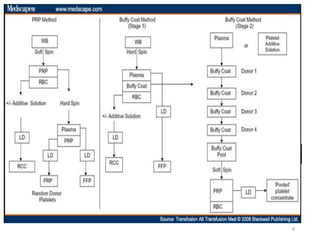
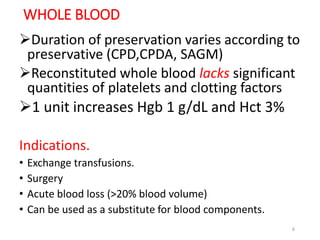
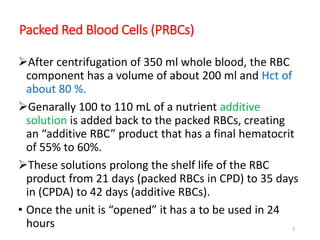
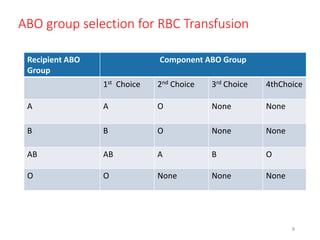
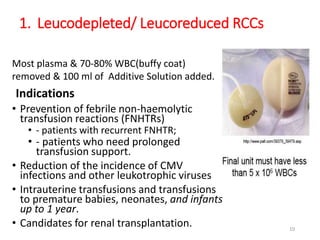
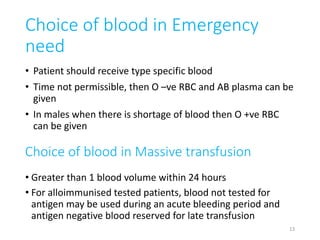
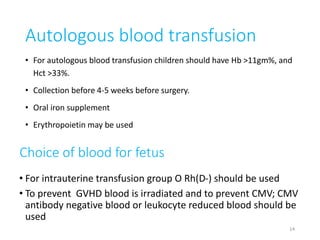
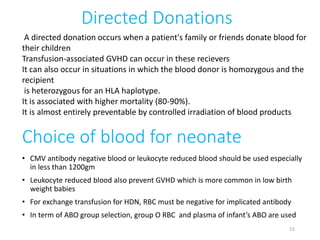
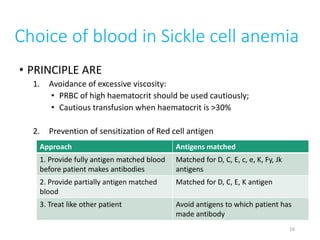
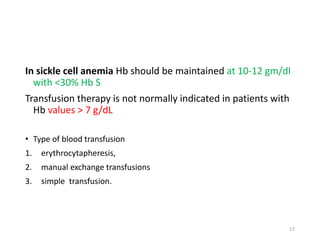
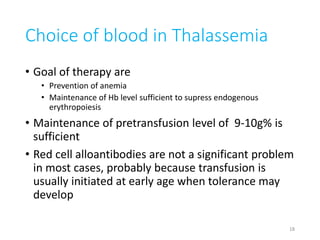
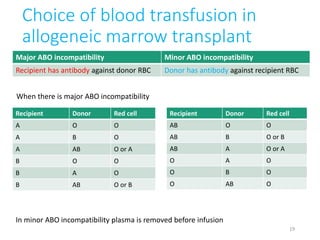
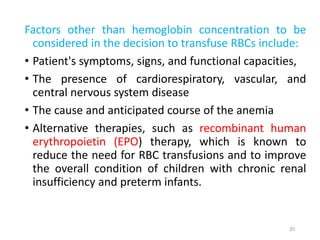
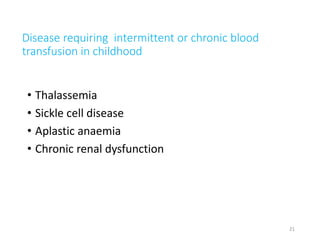
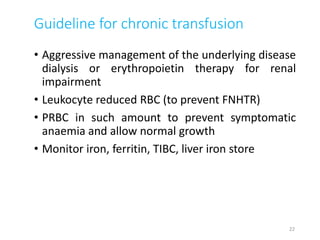
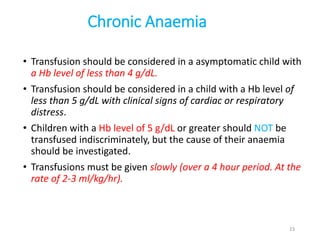
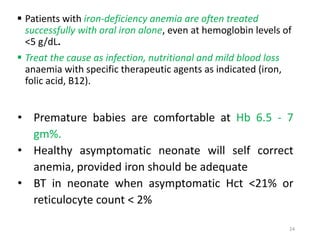
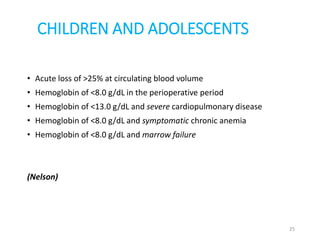
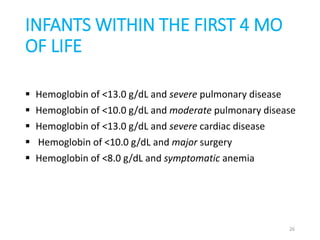
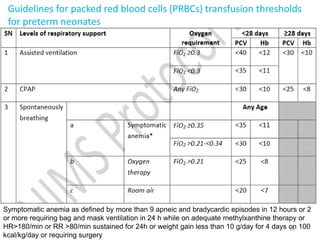
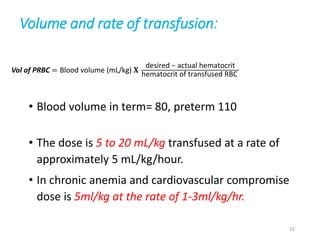
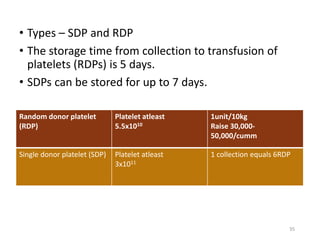
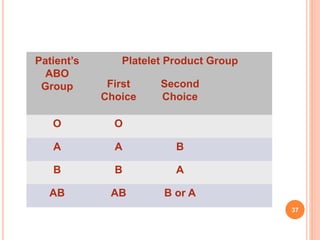
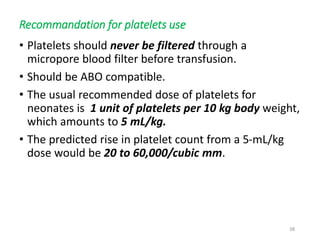
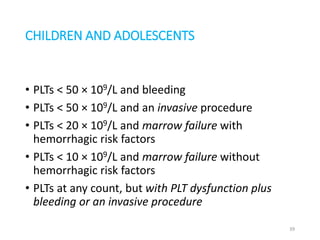
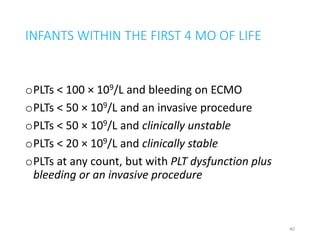
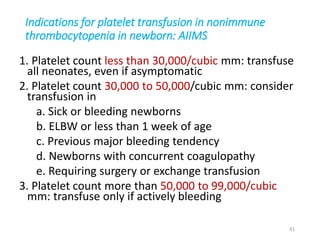
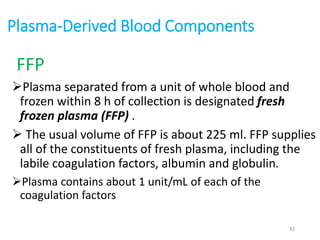
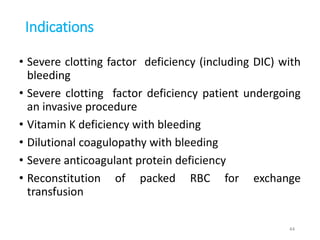
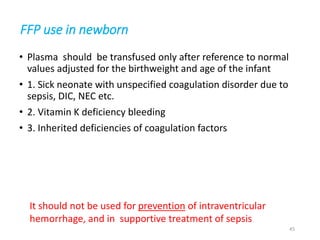
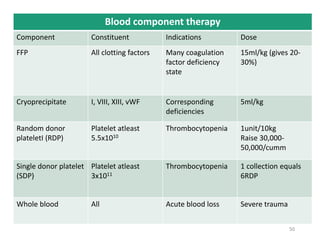
This document provides information about blood and blood component therapy. It discusses the types of blood components that can be derived from whole blood donations, including packed red blood cells, platelet concentrates, and fresh plasma. It also outlines guidelines for choosing appropriate blood components for different patient populations and clinical situations, such as neonates, pediatric patients, and those with diseases like sickle cell anemia or thalassemia that require chronic transfusion support. Selection of blood type and volume for transfusion is discussed based on factors like the patient's symptoms, hemoglobin level, and underlying conditions.