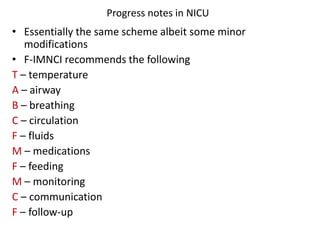
The document provides information on progress notes including:
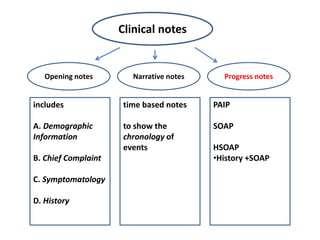
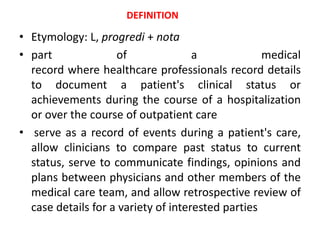
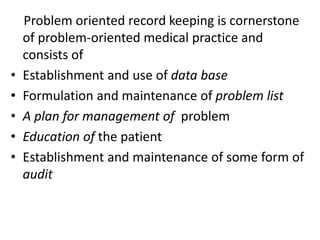
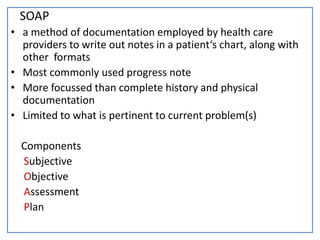
- Progress notes are used to document a patient's clinical status and progress over time during hospitalization or outpatient care.
- They serve to communicate findings between healthcare professionals and allow retrospective review of a patient's case.
- Progress notes are intended to be concise and provide communication about a patient's condition to those accessing their health record. Physicians and nurses are generally required to generate progress notes on a regular basis.