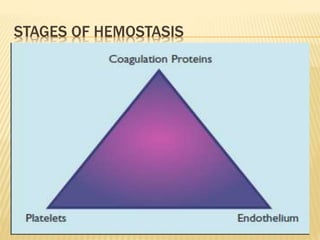
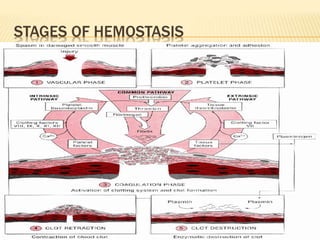
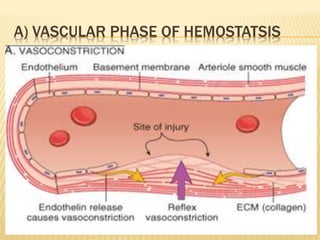
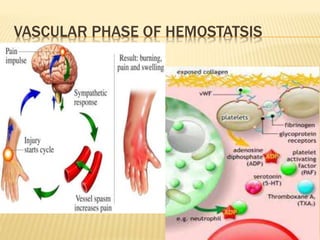
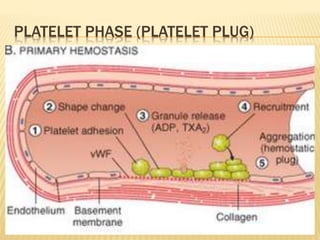
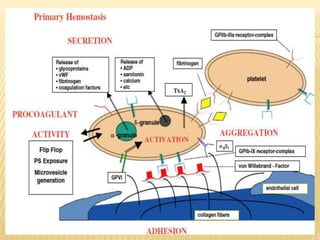
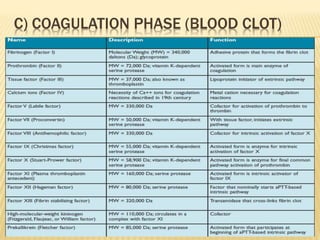
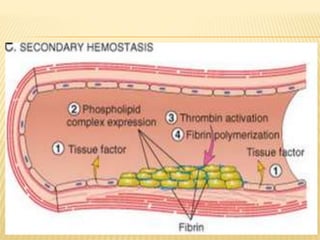
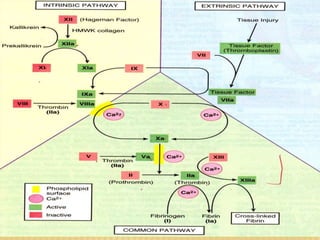
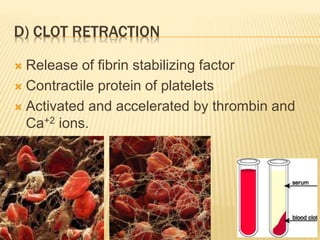
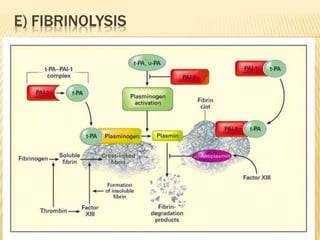
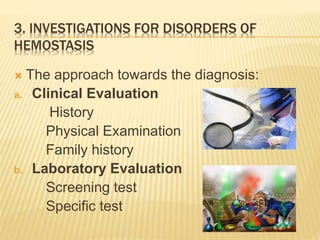
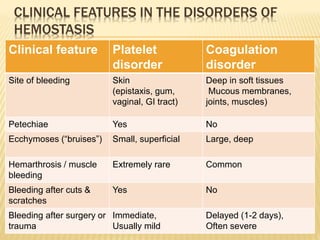
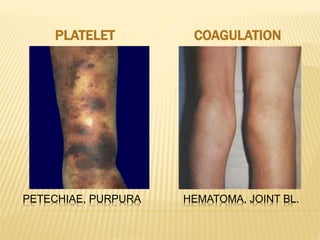
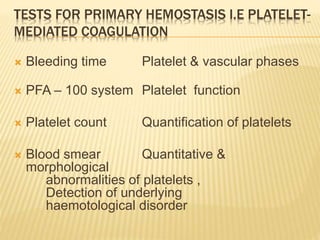
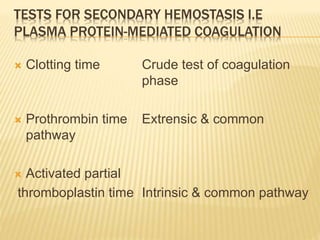
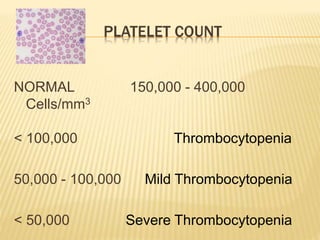
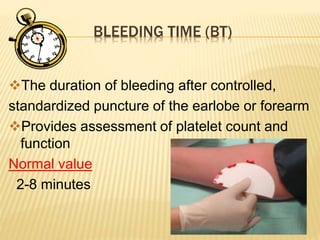
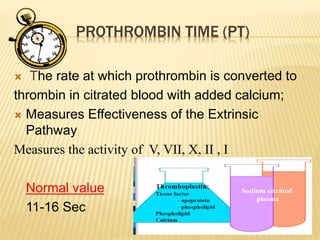
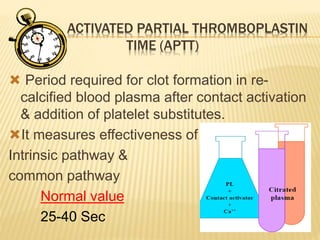
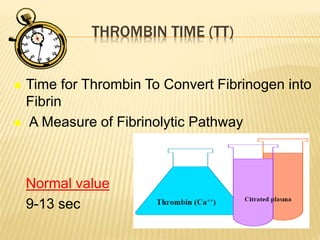
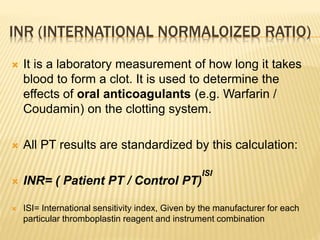
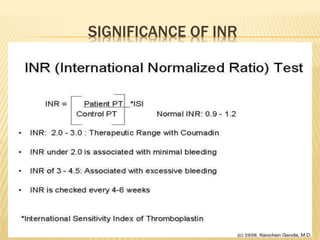
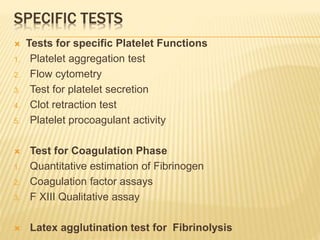
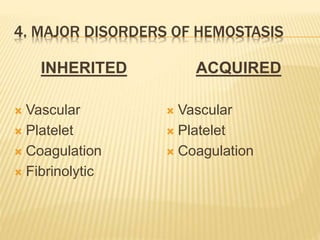
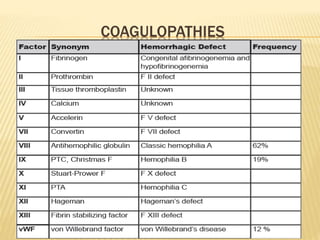
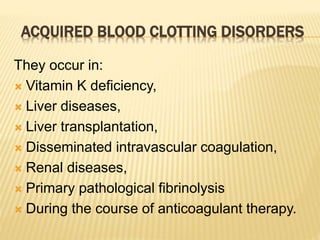
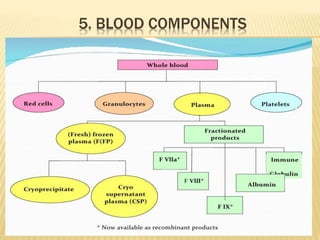
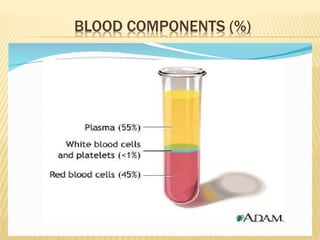
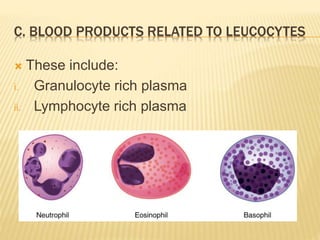
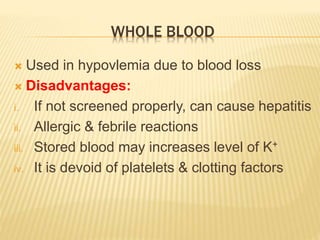
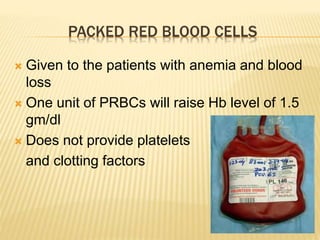
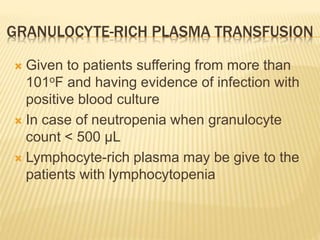
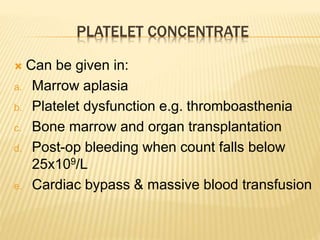
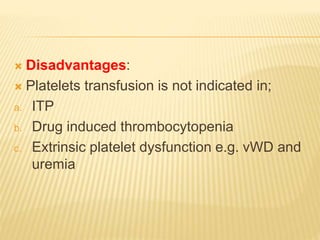
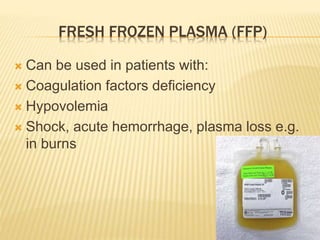
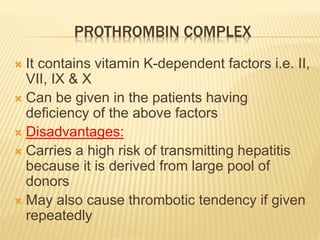
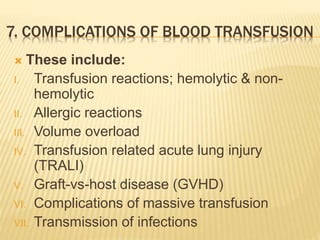
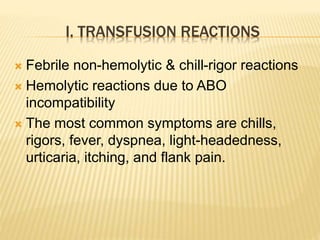
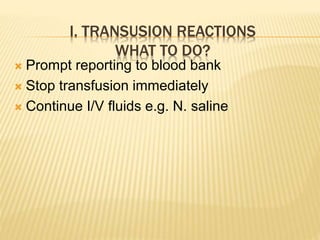
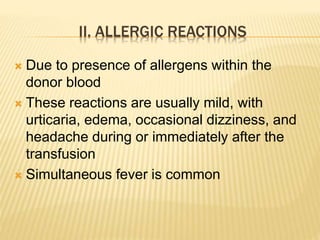
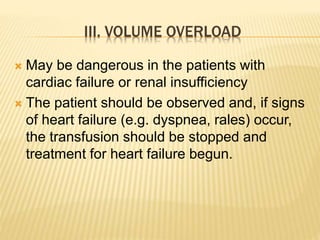
This document discusses hemostasis and blood transfusion. It begins with definitions of hemostasis and describes the five stages of hemostasis: vascular phase, platelet phase, coagulation phase, clot retraction, and fibrinolysis. It then discusses investigations for disorders of hemostasis, including clinical evaluation and laboratory tests. Major disorders of hemostasis are outlined, including inherited and acquired issues with blood vessels, platelets, and coagulation. The document also covers blood components, indications for component therapy, and potential complications of blood transfusion.