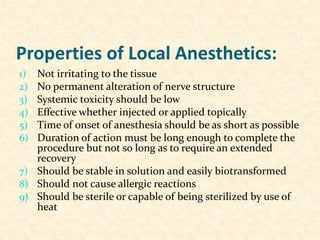
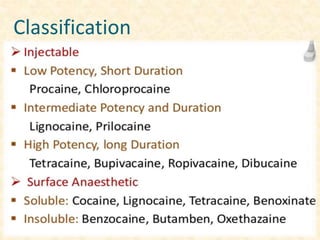
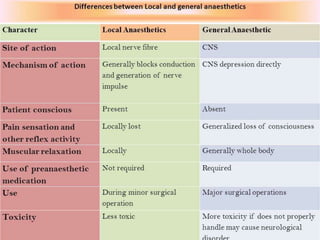
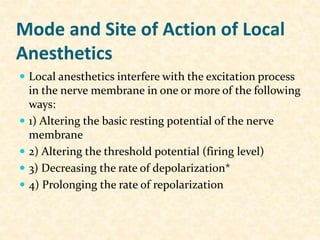
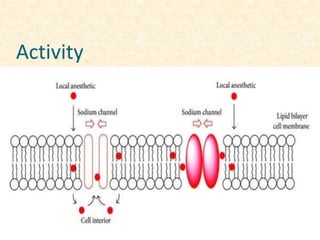
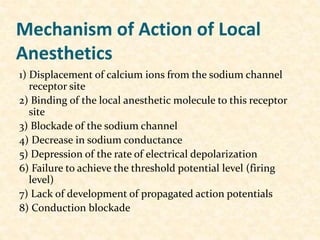
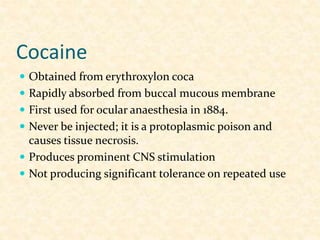
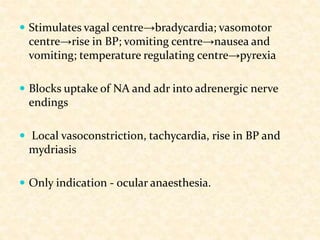
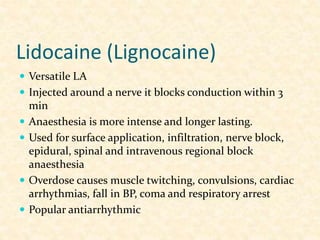
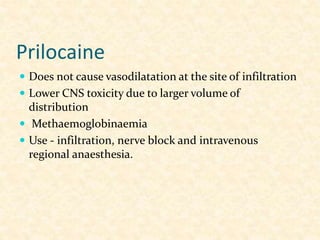
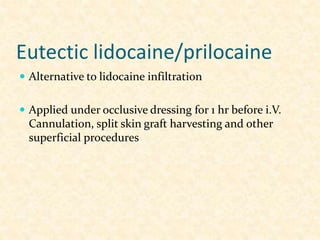
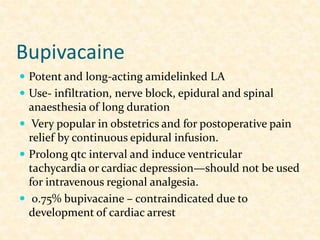
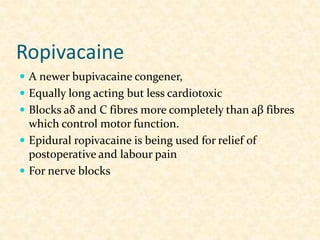
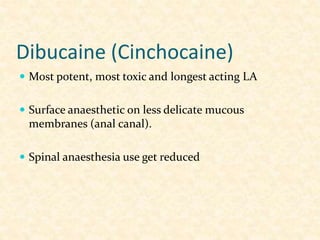
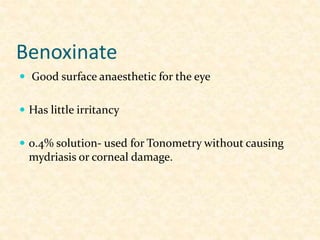
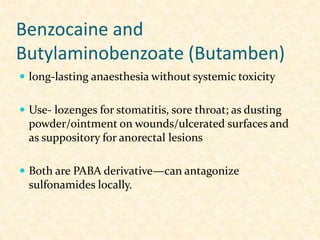
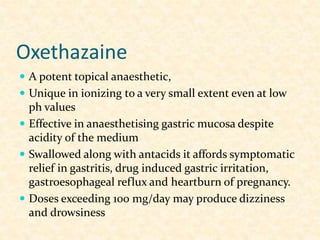
This document defines local anesthetics and describes their properties and mechanisms of action. It discusses various local anesthetics including lidocaine, prilocaine, bupivacaine, ropivacaine, dibucaine, benzocaine, butamben, and oxethazaine. It covers their uses for surface anesthesia, infiltration, nerve blocks, epidurals, and other techniques. Complications are also summarized.