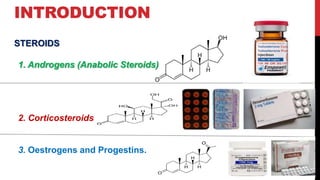
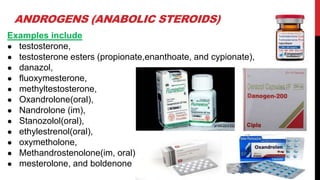
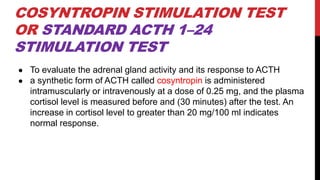
The document discusses the pharmacology of steroids, including anabolic steroids, corticosteroids, estrogens, and progestins, detailing their mechanisms, uses, and adverse effects. Case studies illustrate practical applications of these steroids in clinical settings, along with specific hormone replacement therapies. Adverse effects of steroids range from virilization in women to cardiovascular complications and hormonal imbalances in both sexes.