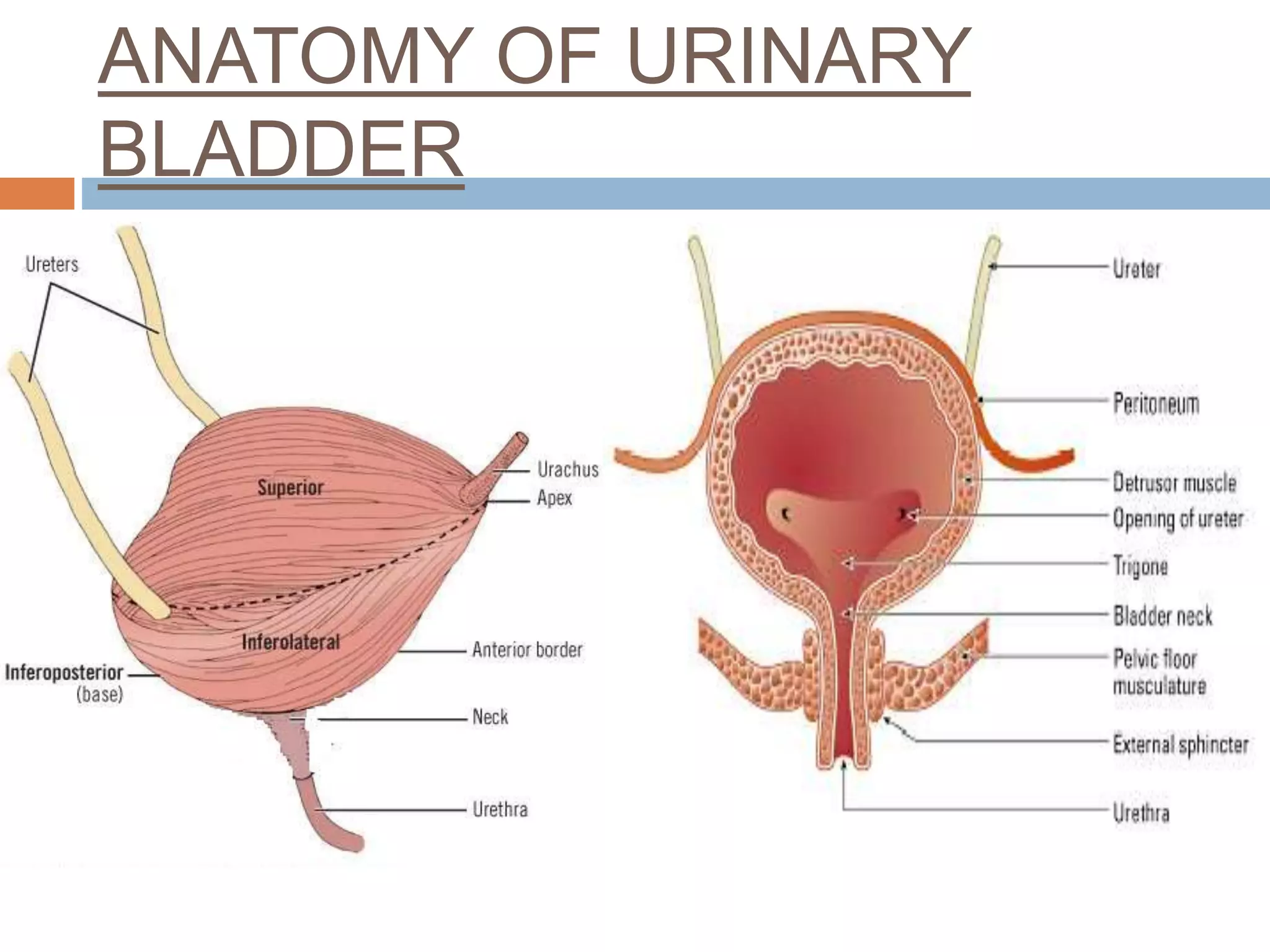
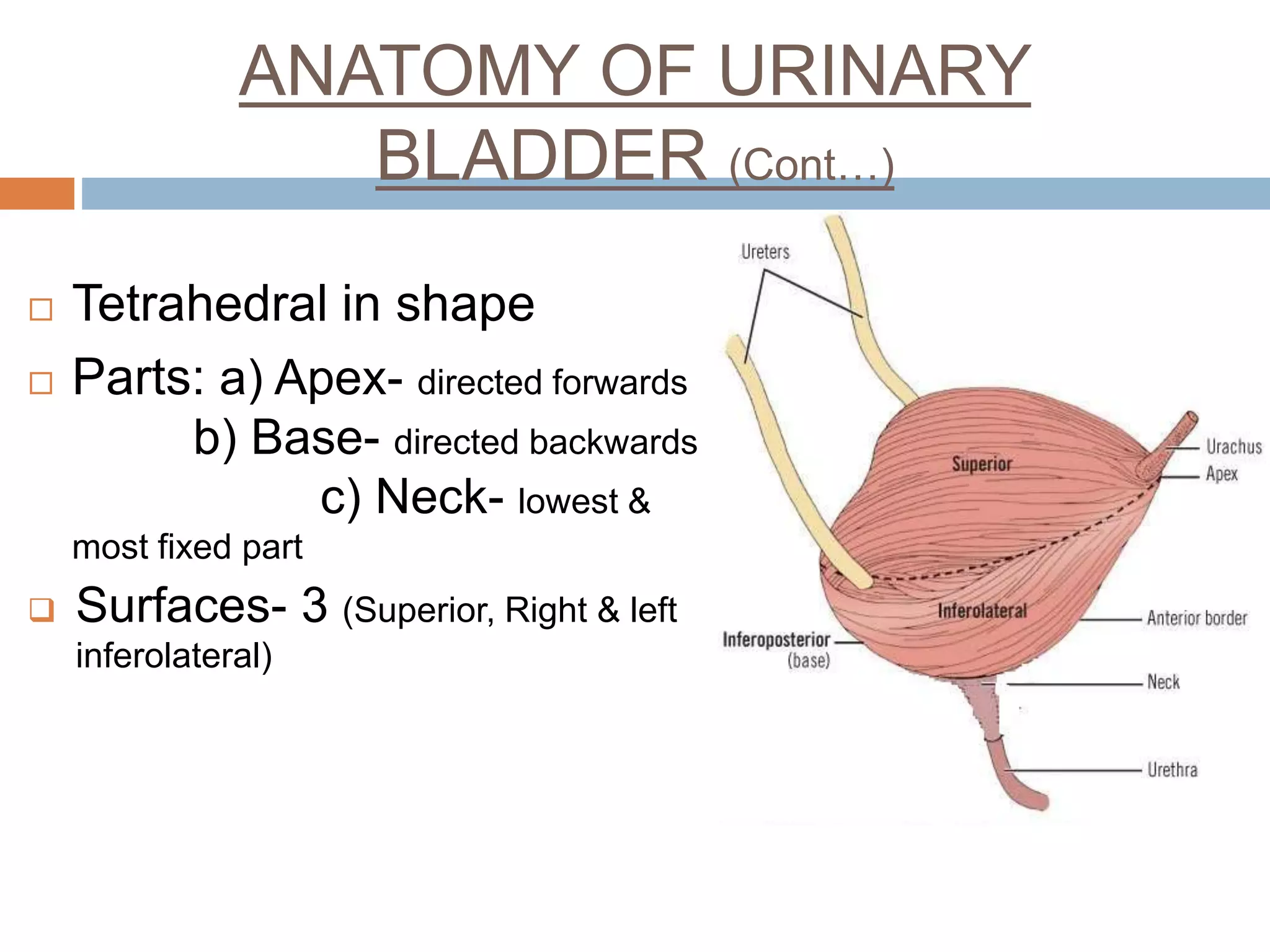
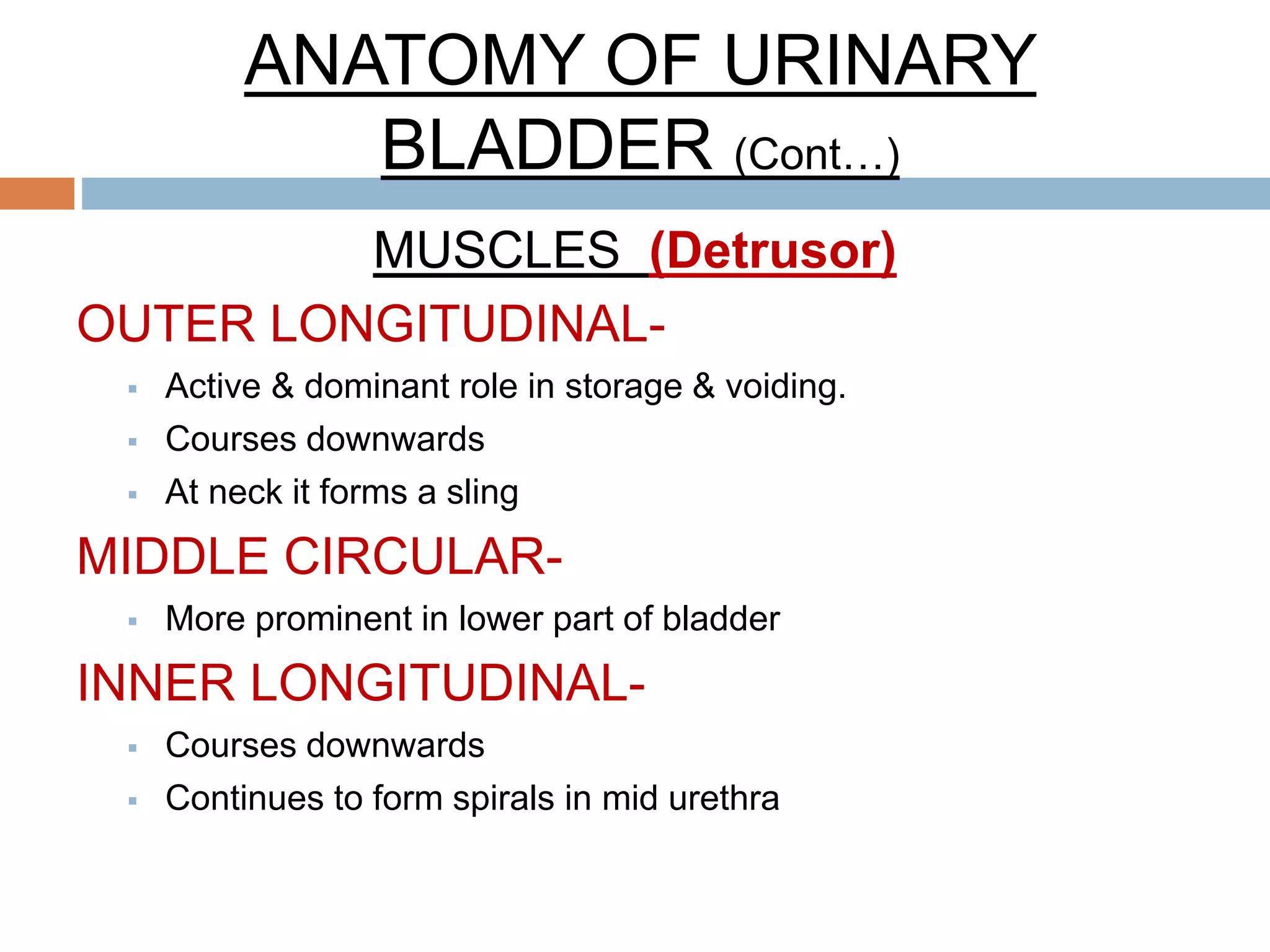
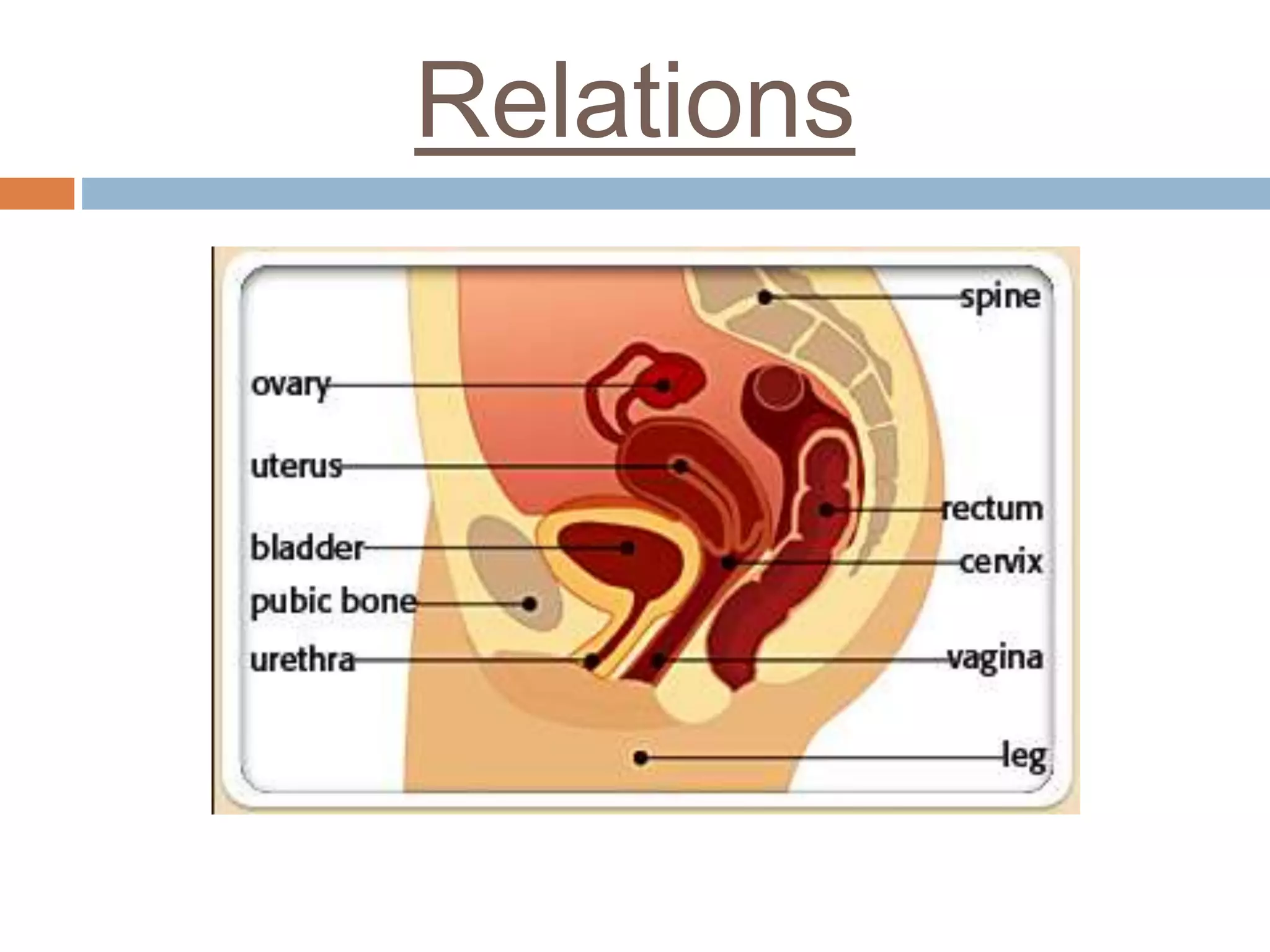
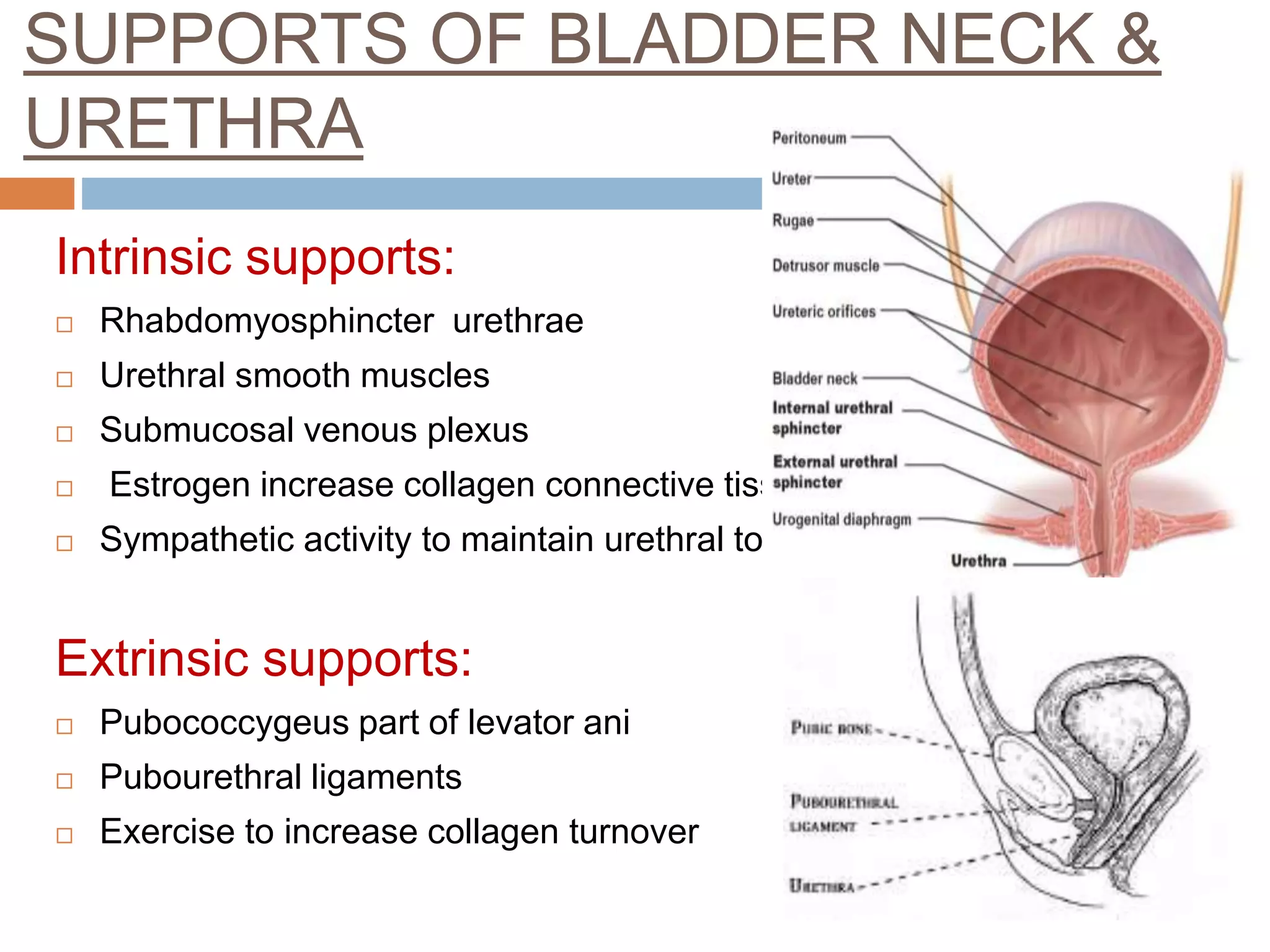
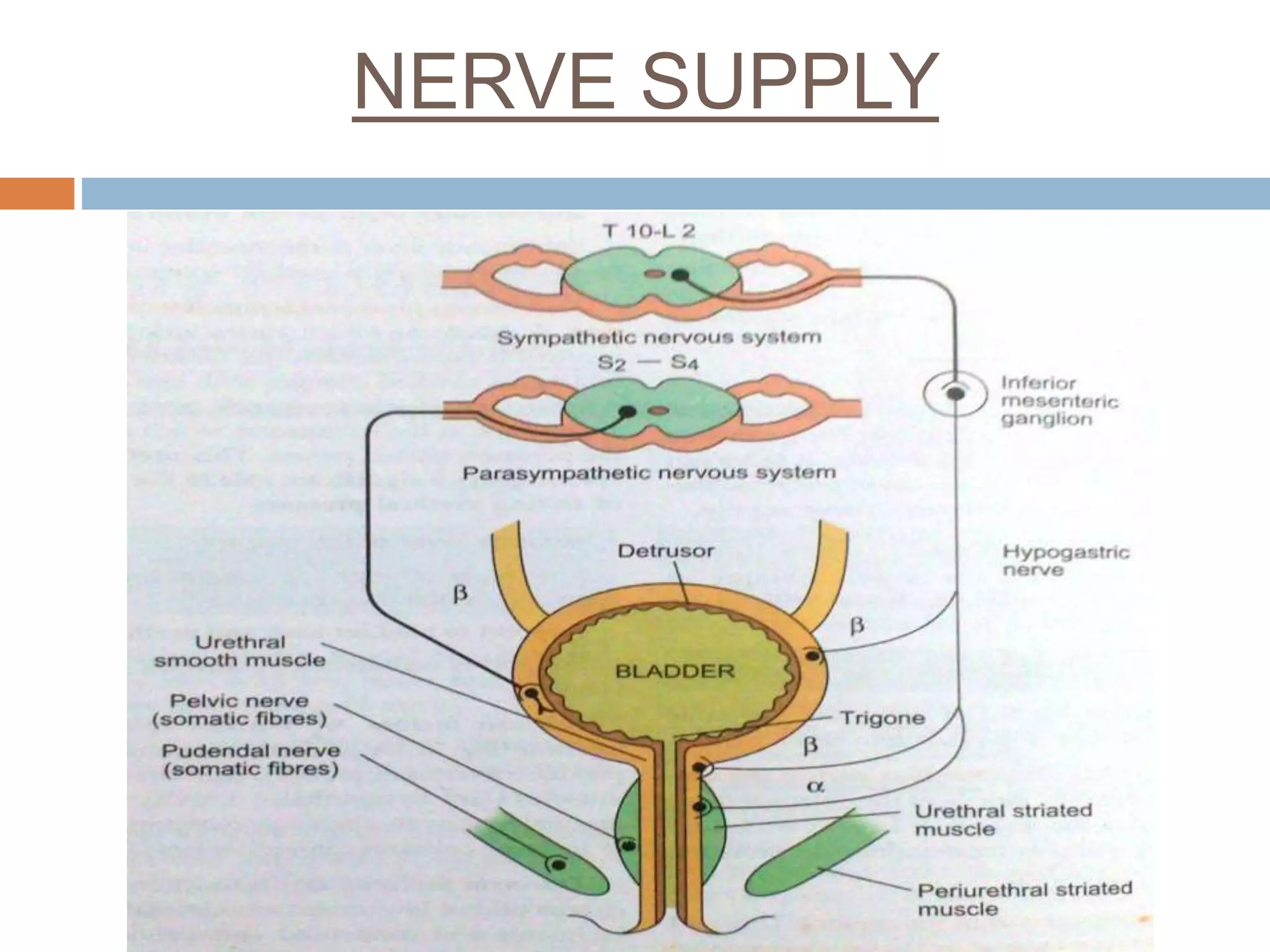
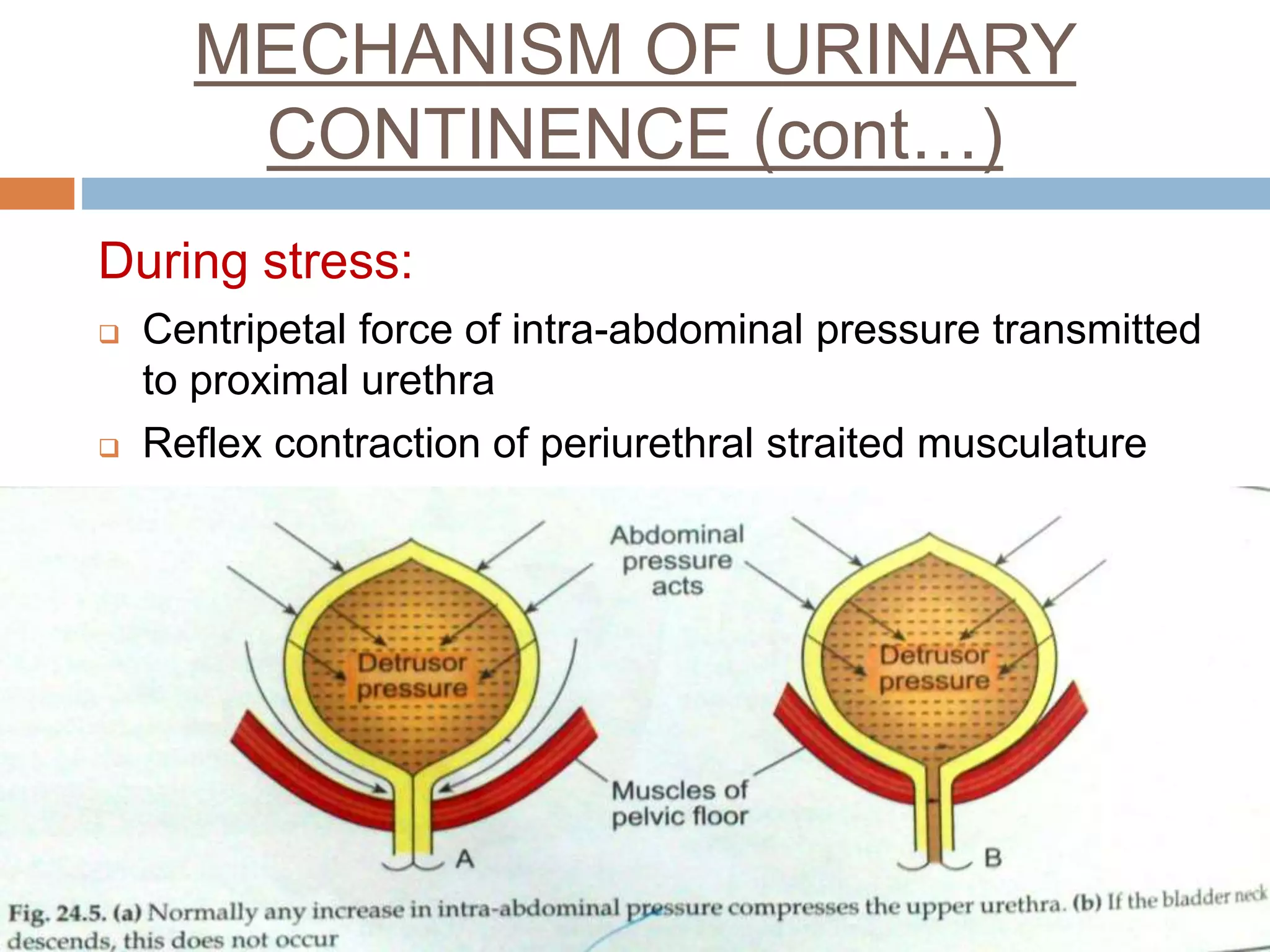
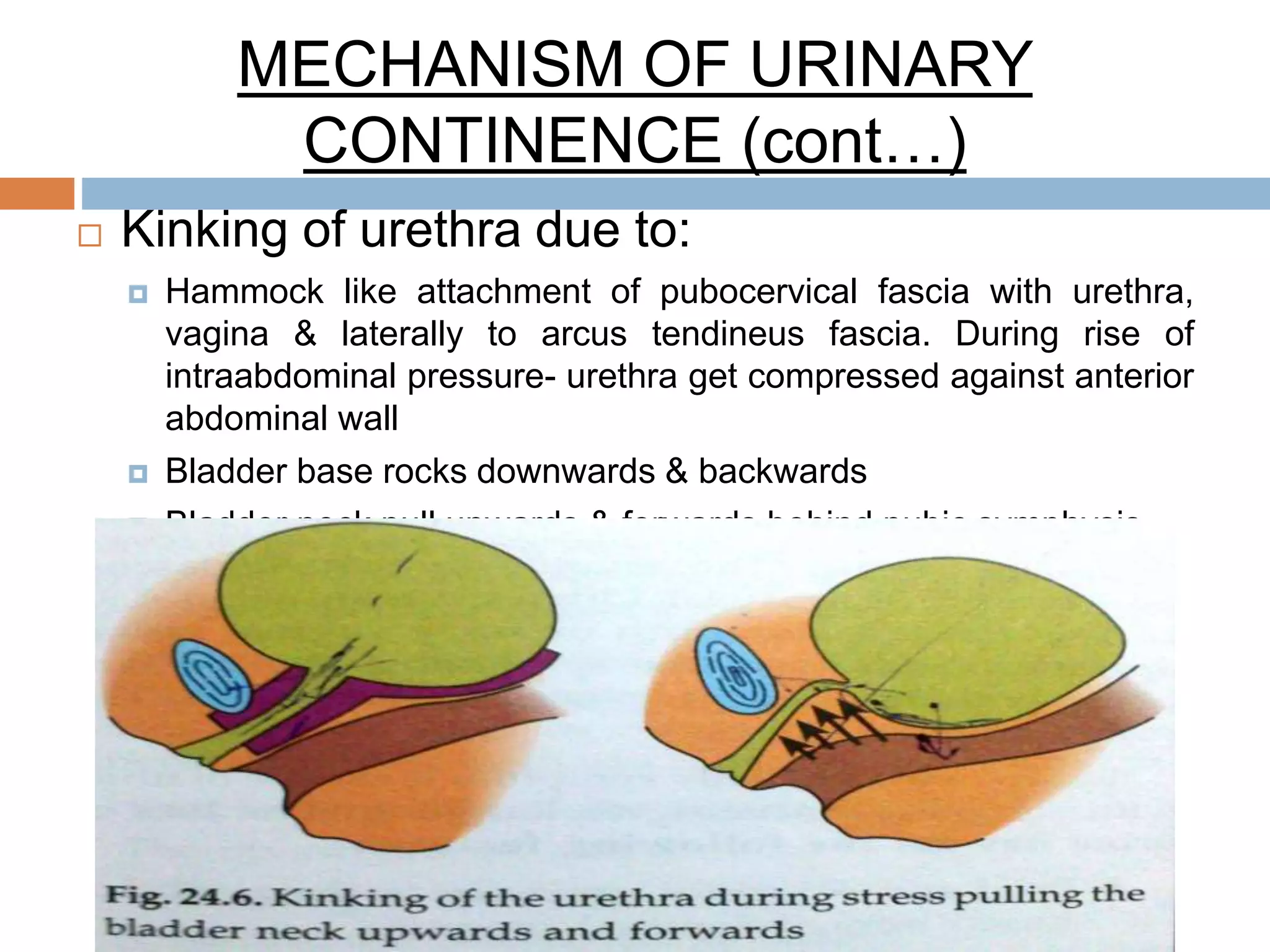
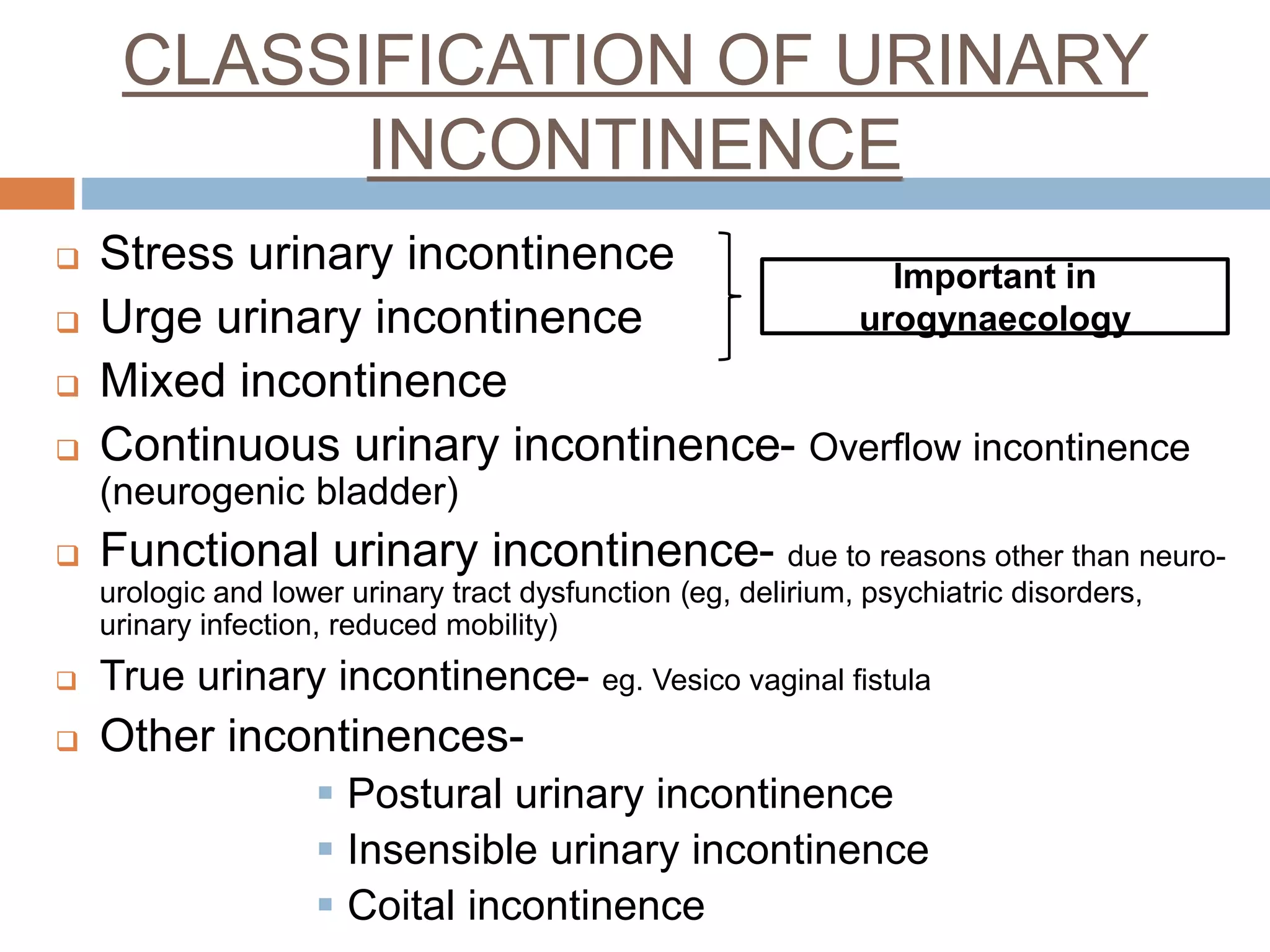
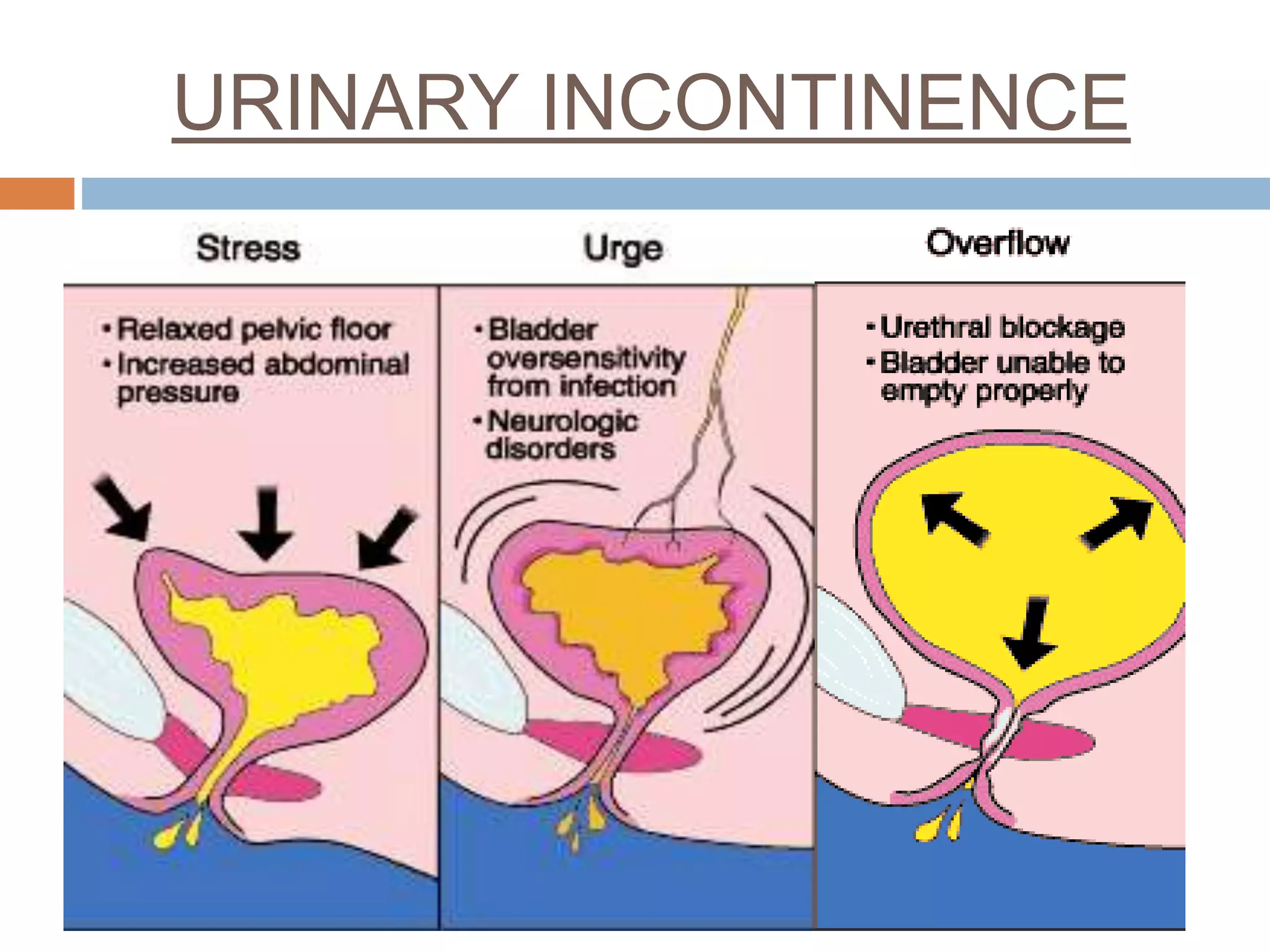
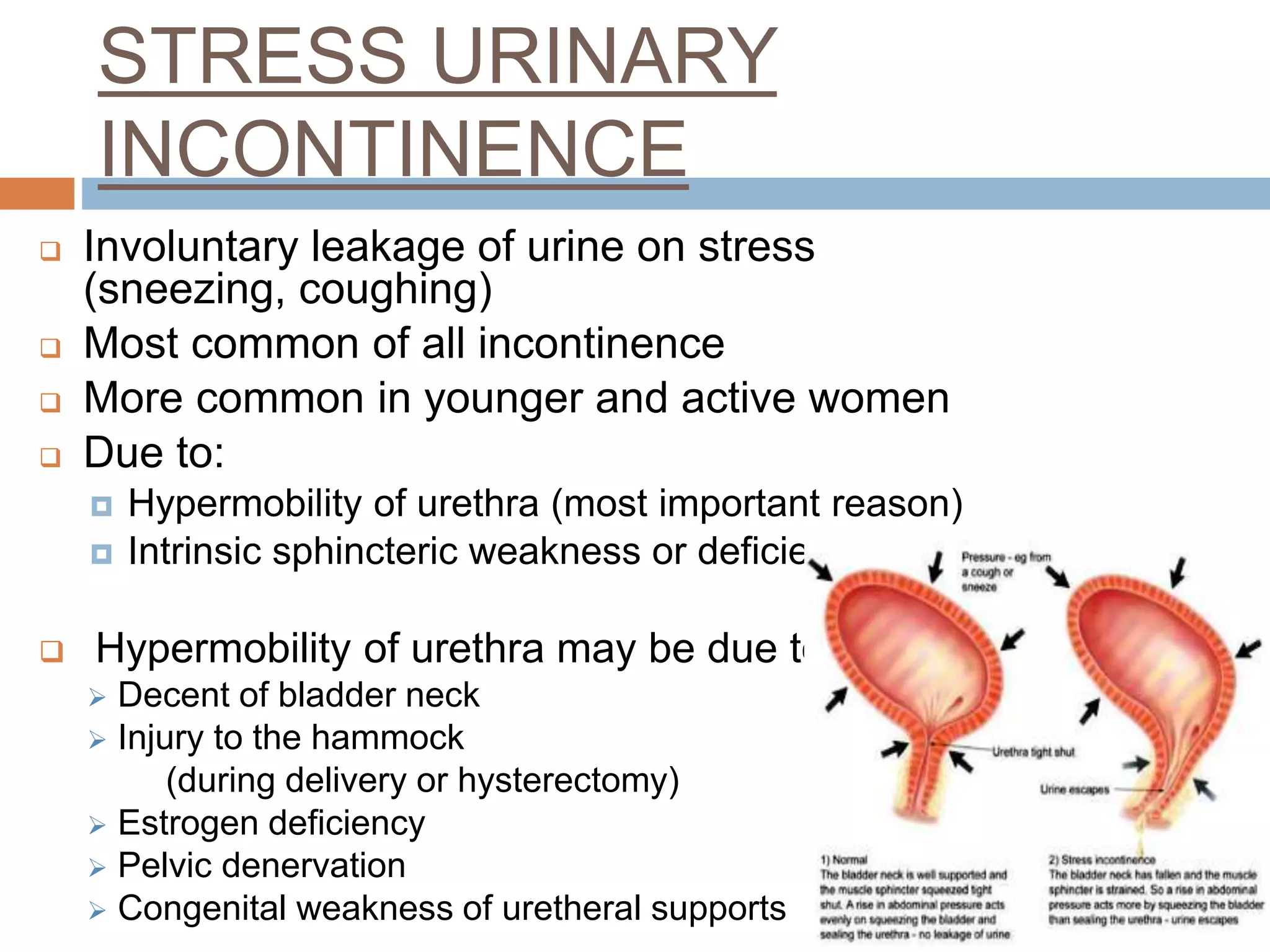
The urinary bladder is a tetrahedral shaped organ located in the pelvis. It has three surfaces and is composed of layers of muscles including the detrusor muscle. During storage, the bladder fills with urine while maintaining low pressure through relaxation of the detrusor and contraction of the internal urethral sphincter. During voiding, the detrusor contracts to increase pressure while the sphincter relaxes to allow urine outflow. Urinary incontinence can be stress-related from urethral hypermobility or urge-related from detrusor overactivity. Treatment depends on the type but may include lifestyle changes, medications, devices, bladder training, or surgery.