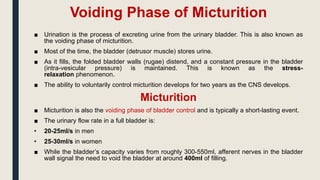
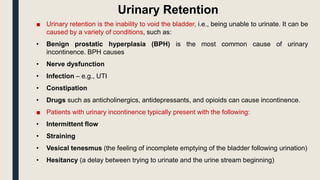
The kidneys filter around 150-180 liters of blood plasma daily but only produce 1-1.8 liters of urine by reabsorbing the rest. Urine contains waste products and is usually yellow and slightly acidic. Micturition is the process of emptying the bladder in two phases - storage and voiding. During storage, the bladder relaxes and fills while sphincters contract to prevent leakage. During voiding, the bladder contracts while sphincters relax to allow urine passage. Nervous system control and any lesions impact the phases' coordination.