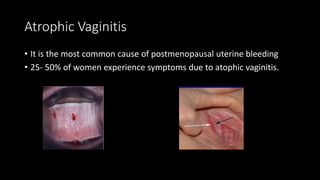
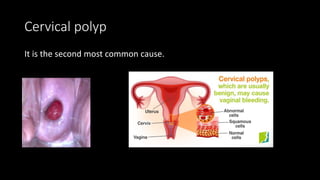
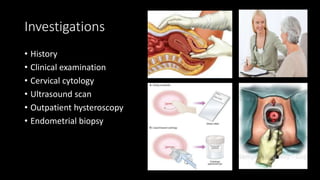
This document discusses postmenopausal bleeding, defined as any vaginal bleeding occurring more than 12 months after a woman's last menstrual period. The most common causes are atrophic vaginitis (60-80%), estrogen treatments (15-25%), and cervical or uterine polyps (2-12%). Evaluation involves obtaining a medical history, performing a clinical examination including a cervical smear and pelvic exam, and diagnostic testing such as ultrasound and endometrial biopsy. Treatment depends on the underlying cause, but may include hormone therapy for atrophic vaginitis or polyp removal, and in some cases of hyperplasia or cancer, hysterectomy.