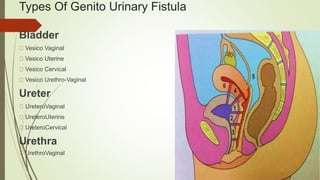
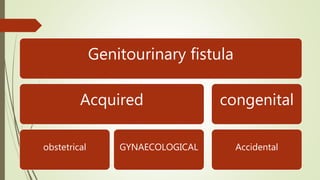
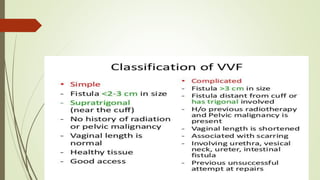
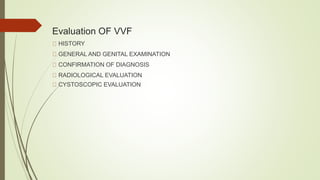
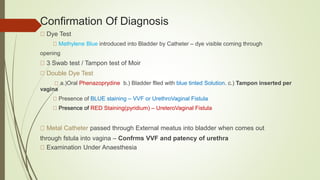
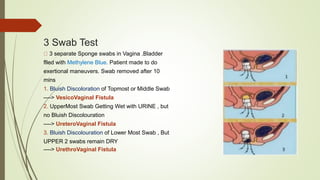
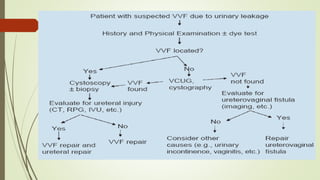
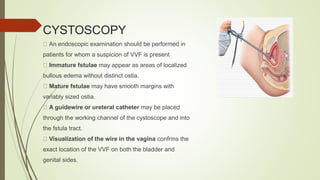
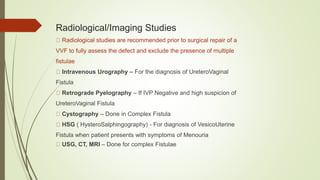
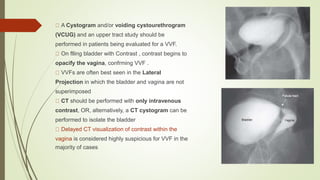
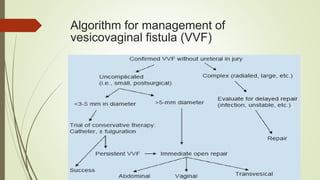
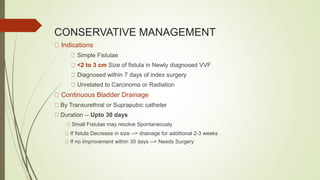
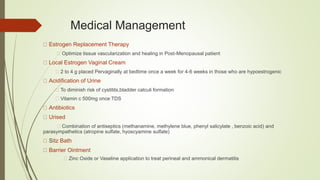
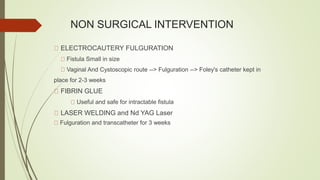
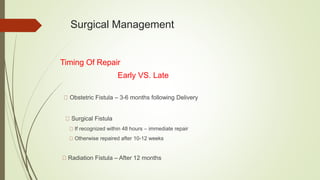
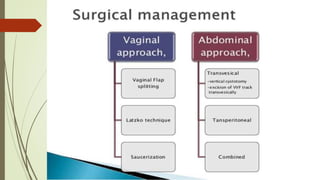
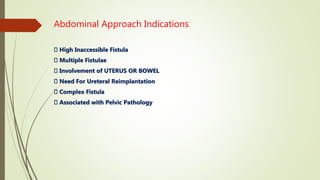
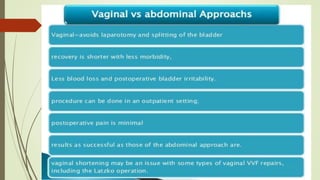
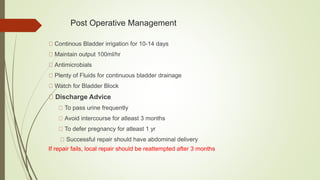
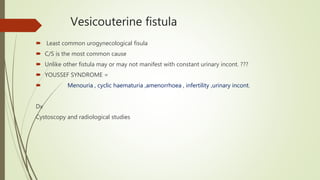
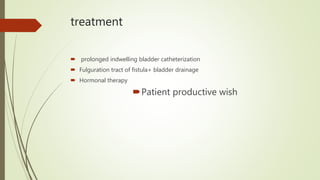
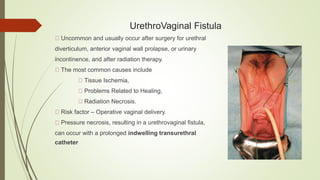
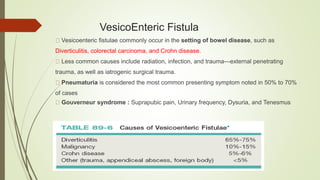
Urinary tract fistulas can occur between the urinary tract and other organs. The most common type is a vesicovaginal fistula, which is an abnormal connection between the bladder and vagina causing involuntary urine leakage. Causes include prolonged obstructed labor, pelvic surgery, radiation therapy, and trauma. Diagnosis involves dye tests and imaging. Treatment depends on the type and cause but may include conservative management, surgery to repair the fistula, or in some cases, nephrectomy.